Photo by Mike Seyfang (Flickr Creative Commons)
The Fox news piece, “Marijuana-like brain chemicals could be key to treating Fragile X syndrome”, highlighted an original research article, by Drs. Daniele Piomelli and Olivier Manzoni and colleagues, that found boosting the production of a natural marijuana-like chemical in the brain, 2-AG, called an endocannabinoid, could restore normal brain function and behavior in the mouse model of Fragile X.
Although this finding is very exciting, don’t make the marijuana brownies just yet!
A subsequent research article, published in Nature Medicine (Busquets-Garcia et al, May, 2013) came to the opposite conclusion. The study found that blocking the action of endocannabinoids, like 2-AG, was therapeutic in the Fragile X mouse. 2-AG is a chemical messenger, called a neurotransmitter, which is produced in one brain cell (Cell X) and then travels to another brain cell (Cell Y) where it activates Cell Y by interacting with a protein on the surface of Cell Y called a receptor.
The Busquets-Garcia study found that a blockade of the 2-AG receptor, called cannabinoid 1 receptor (CB1R), with an antagonist, restores normal behaviors, brain function and anatomy in Fragile X mice.
So, what’s going on?
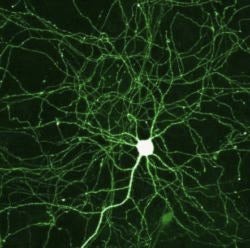
Studies in the Fragile X mouse have shown that depending on the brain region and the cell type, the function of the endocannabinoid messenger can either increase or decrease. Brain cells or neurons come in two major types, excitatory neurons, which “excite” or increase electrical activity in the brain, and inhibitory neurons, which “inhibit” or dampen electrical activity.
A finely tuned balance of excitatory and inhibitory neuron function is essential for normal brain activity. When an imbalance occurs, for example, with too much excitatory neuron function or too little inhibitory neuron function, epilepsy can result. Because epilepsy is more common in Fragile X patients, one theory is that there is an imbalance in excitatory and/or inhibitory neuron function.
Interestingly, in the mouse Fragile X brain, the effects of 2-AG on inhibitory neurons is actually increased (Zhang and Alger, J. Neuroscience, 2010; Maccarrone, et al., Neuropsychopharmacology, 2010), but if the target cell of 2-AG is an excitatory neuron, then the effects of 2-AG are decreased, as shown in the Piomelli and Manzoni study.
In addition to different cell types, each of these studies measured endocannabinoid function in different brain regions of Fragile X mice. So, it is possible that endocannabinoid function is affected differently in different brain regions.
What to do now?
There is a consensus that endocannabinoid function is changed in Fragile X, and this promises to be a fruitful avenue for development of new therapeutics.
Because the direction of change of endocannabinoid function in Fragile X depends on other factors, specific behaviors may be helped by boosting endocannabinoids while other behaviors or symptoms may be unaffected or made worse.
Future research efforts in animal models are aimed at trying to determine if there are different molecular mechanisms of endocannabinoid function at inhibitory and excitatory neurons and to understand why they are differently affected in Fragile X. Results of such studies may allow the development of therapeutics that selectively inhibit endocannabinoid function at inhibitory neurons, but boost it at excitatory neurons.
Author
 Kim Huber, PhD
Kim Huber, PhDis a renowned scientist who has played a key role in advancing our understanding of Fragile X syndrome. Her research has been critical to recent breakthroughs leading to the development of potential new treatments (currently undergoing clinical trials) that address the core deficits in FXS. Kim has a deep awareness of and sensitivity to how her research ultimately impacts families. As a result, she played a role in the establishment of the Fragile X Clinic in Dallas, Texas.

