Newly Diagnosed
We are here to help you. When you’re ready, there is a whole community that understands what you’re going through, and will be here to provide guidance and support throughout your journey.
Newly Diagnosed
We are here to help you. When you’re ready, there is a whole community that understands what you’re going through, and will be here to provide guidance and support throughout your journey.
You Are Not Alone
Your child has been diagnosed with Fragile X syndrome. While this is difficult news, we’re so glad you’ve found us.
We have a lot of information to share with you.
- You and Your Child
First, you need to breathe. This is happening, and in time you’re going to need to work toward acceptance. Take the time now to love your child and focus on your self-care. - Accessing Services
Your child has a right to free, public education that meets their unique needs from birth through to age 21. Learn where and how to connect to your state’s services. - Visit a Fragile X Clinic
These are clinics with expertise specific to your child’s condition. Skip the “What’s Fragile X?” questions and instead find a safe place with the support you need. - See a Genetic Counselor
You can find a genetic counselor many ways, including through a Fragile X clinic, but why is this important? Learn why and what to expect. - Telling Others
There are many reasons to know how to explain Fragile X to others, including talking to your “typical” children and informing relatives of possible carrier issues. - How to Reach Us
The different ways you can reach us and others in the Fragile X community. Real people are here for you!
The first thing we want you to know is: You can contact us at any time , and we encourage you to do so.
The NFXF was founded nearly 40 years ago and as long as Fragile X disorders exist, we’re not going anywhere. Think of us as your shoulder to lean on, and your safe place where you can always be yourself.
“Hang in there. There is a lot of help out there — seek it out. It can be a roller coaster at times but so worth it.”
—a fragile x mom
The Fragile X community is made up of parents and families just like you. Knowing that there are others impacted by Fragile X out in the world who share your challenges and triumphs can be incredibly empowering … when you’re ready.
Whether you’re the child’s mother, father, grandparent, friend … we first want you to breathe. Then give your newly diagnosed child lots of hugs and kisses. Then focus on your self-care.
Then, when you’re ready, we’ll be here for everything else.
 Let’s Make Sure You’re in the Right Place
Let’s Make Sure You’re in the Right Place
This resource is designed to help parents who have a child with a new diagnosis of Fragile X syndrome, which is one of three main Fragile X disorders.
If this doesn’t describe you, you might be looking for information on a new diagnosis for:
Fragile X–associated tremor/ataxia syndrome — also referred to as FXTAS and pronounced fax-tass — is an “adult onset” neurodegenerative disorder, usually affecting males over 50 years of age. Females comprise only a small part of the FXTAS population, and their symptoms tend to be less severe. FXTAS affects the neurologic system and progresses at varying rates in different individuals. Learn more:
Fragile X–associated primary ovarian insufficiency — also referred to as FXPOI, and pronounced fax-poy — is a condition in which the ovaries are not functioning at full capacity in an FMR1 premutation carrier.
FXPOI occurs in about 20-25% of adult female FMR1 premutation carriers. It has also been reported in teenagers who are carriers, though it is less common in that population. Learn more:
When you or someone in your family are told you are a “carrier” for a Fragile X mutation, many questions arise. Do you have a premutation or full mutation? What does it mean for your health, your family, and your future? Does the size of your FMR1 gene matter? Learn more:
Also see information for FXTAS and FXPOI.
 Let’s Make Sure You’re in the Right Place
Let’s Make Sure You’re in the Right Place
This resource is designed to help parents who have a child with a new diagnosis of Fragile X syndrome, which is one of three main Fragile X disorders.
If this doesn’t describe you, you might be looking for information on a new diagnosis for:
Fragile X–associated tremor/ataxia syndrome — also referred to as FXTAS and pronounced fax-tass — is an “adult onset” neurodegenerative disorder, usually affecting males over 50 years of age. Females comprise only a small part of the FXTAS population, and their symptoms tend to be less severe. FXTAS affects the neurologic system and progresses at varying rates in different individuals. Learn more:
Fragile X–associated primary ovarian insufficiency — also referred to as FXPOI, and pronounced fax-poy — is a condition in which the ovaries are not functioning at full capacity in an FMR1 premutation carrier.
FXPOI occurs in about 20-25% of adult female FMR1 premutation carriers. It has also been reported in teenagers who are carriers, though it is less common in that population. Learn more:
When you or someone in your family are told you are a “carrier” for a Fragile X mutation, many questions arise. Do you have a premutation or full mutation? What does it mean for your health, your family, and your future? Does the size of your FMR1 gene matter? Learn more:
Also see information for FXTAS and FXPOI.
You Are Not Alone
Your child has been diagnosed with Fragile X syndrome. While this is difficult news, we’re so glad you’ve found us.
We have a lot of information to share with you.
The first thing we want you to know is: You can contact us at any time , and we encourage you to do so.
The NFXF was founded nearly 40 years ago and as long as Fragile X disorders exist, we’re not going anywhere. Think of us as your shoulder to lean on, and your safe place where you can always be yourself.
“Hang in there. There is a lot of help out there — seek it out. It can be a roller coaster at times but so worth it.”
—a fragile x mom
The Fragile X community is made up of parents and families just like you. Knowing that there are others impacted by Fragile X out in the world who share your challenges and triumphs can be incredibly empowering … when you’re ready.
Whether you’re the child’s mother, father, grandparent, friend … we first want you to breathe. Then give your newly diagnosed child lots of hugs and kisses. Then focus on your self-care.
Then, when you’re ready, we’ll be here for everything else.
- You and Your Child
First, you need to breathe. This is happening, and in time you’re going to need to work toward acceptance. Take the time now to love your child and focus on your self-care. - Accessing Services
Your child has a right to free, public education that meets their unique needs from birth through to age 21. Learn where and how to connect to your state’s services. - Visit a Fragile X Clinic
These are clinics with expertise specific to your child’s condition. Skip the “What’s Fragile X?” questions and instead find a safe place with the support you need. - See a Genetic Counselor
You can find a genetic counselor many ways, including through a Fragile X clinic, but why is this important? Learn why and what to expect. - Telling Others
There are many reasons to know how to explain Fragile X to others, including talking to your “typical” children and informing relatives of possible carrier issues. - How to Reach Us
The different ways you can reach us and others in the Fragile X community. Real people are here for you!
1. You and Your Child
Remember to Breathe
“Getting a diagnosis is hard. It’s really hard. There has been nothing else like it in my life and I cannot imagine there ever will be. It made me sad . . . really sad.”
—Jayne Dixon Weber
Your mind and body need breaks, and adding a few minutes of deep breathing to your daily routine can make a difference. What you’re going through right now is hard . . . and confusing and overwhelming . . . and you’re perfectly normal if you’re also feeling angry, bitter, guilty, afraid — of the knowns and the unknowns — and yes, sad.
If you’re feeling anxious or overwhelmed right now, take a slow, deep breath . . . in through your nose, focusing on the incoming air filling your belly . . . then a slow exhale out through your nose.
On the next breath, place one hand on your belly and one on your chest. Take another slow deep breath in through your nose, this time focusing on the feel of your belly rising, then your chest (just a little), and exhale out your nose, emptying your chest first, then your belly. Repeat three times.
Also watch our webinar from psychologist and research scientist Anne Wheeler: Using Mindfulness and Acceptance Techniques to Reduce Stress and Improve Coping↗.
Make Self-Care a Priority
We humans tend to ignore self-care during a crisis, but focusing on your physical and mental health right now can lessen your stress and anxiety in the long run. We can’t stress this enough.
Part of your job of caring for your child is caring for yourself. Think of like when you’re a passenger on an airplane, and the flight attendant instructs you to put the oxygen mask on yourself before you put one on your child.
If you’re not there, who will put their mask on?
The emotions you’re going through right now are intense and new. How long they last will vary, and rather than ignoring them, try to acknowledge them. We promise, the intensity will lessen.
Signs of Caregiver Stress
- Feeling overwhelmed
- Feeling sad
- Constant worrying
- Feeling tired most of the time
- Getting too much sleep
- Not getting enough sleep
- Gaining weight
- Losing weight
- Easily angered or irritated
- Loss of interest in things you used to enjoy
- Frequent headaches or other physical pain
- Abusing alcohol and other drugs
Tips for Managing Stress
- Accept help
- Focus on what you can provide to your child (no one’s perfect)
- Set realistic goals and break them down into smaller tasks
- Connect with others in your social circle, support groups, and resources to streamline some of your responsibilities
- Set healthy goals for yourself
- See a doctor or therapist
Read more from the Mayo Clinic on “Caregiver stress: Tips for taking care of yourself”↗
Find a Therapist↗ is a tool from Psychology Today. If your emotions continue to feel overwhelming, this will help you find a local (or by teletherapy) therapist, psychiatrist, or treatment center near you.
When Your Doctor Says “I Have Bad News”↗ from Jessie Gruman, who has interviewed hundreds of people who have dealt with serious diagnoses, and she has survived four cancer scares herself. She asserts that even though a scary diagnosis can turn your world upside down, there are practical strategies you can use to take the best next steps and bring balance back to your life.
Gaiam’s YouTube channel↗ offers an amazing number of videos and playlists in categories like yoga, meditation, fitness, and discovery. No matter how much time you have, you can find one that fits your schedule.
Yoga With Adriene↗ offers a 30-day yoga course on YouTube. Day one is learning breathing techniques and moves into poses, stretches, and cool downs.
How to Start and Write a Journal↗ breaks down the steps you can take to keep your thoughts organized and your mind clear through regular journaling.
10 Podcasts for Anxiety↗ provides a curated list of podcasts on dealing with anxiety, including tools, tips, and relaxation techniques.
How to Use Drawing as a Coping Tool for Anxiety↗ lays out the benefits of drawing, plus easy exercises and tips and tricks to get you started.
Learning to Observe and Accept Your Emotions↗ from Verywell Mind.
Reach out to the National Fragile X Foundation: See the form on this page, or:
- Email: treatment@fragilex.org
- Phone: (800) 688-8765
Hug Your Child
At the end of the day remember that your child is still the same wonderful, unique child you’ve loved since they were born. The diagnosis didn’t change that.
What will change is you’ll learn about things you never knew existed. You’ll become a more understanding person. You’ll develop a love for your child that will amaze you. Your child learns differently than you do, but they can and will learn — with your help.
Two Letters
We have two letters to share with you.
The first one is from Avi’s mom. We often ask parents for their advice for newly diagnosed parents, and she wrote this just seven months after Avi’s diagnosis. This is Avi.

My advice for newly diagnosed families is to first allow yourself permission to grieve; to mourn the life you had imagined for your child, the life you had imagined for your family, the hopes and dreams that you had envisioned.
Understand that it is okay to feel whatever you’re feeling; to be sad, angry, worried, lost, and confused.
Then, begin reaching out to other families who understand what you’re going through. Join a Community Support Network↗ near you.
Be leery of the internet. While it can be a tool of knowledge, it can also be a tool of misinformation and negativity.
Know that support from friends and family is important, but, no matter how they try, they may never understand or “get it.”
The grief comes and goes in waves. We only found out 7 months ago, and I am still constantly cycling between anger, hopelessness, sadness, empowerment, strength, courage, hope, and then anger again.
Most days though are days of strength and courage because there’s no other choice. My sweet boy needs a strong mama who can spread awareness, advocate for his needs, be a voice for him since he hasn’t quite found his yet, roll cars and trucks back and forth for what seems like hours, and give unlimited hugs and kisses.
A diagnosis can drive treatment and intervention, but at the end of the day remember that your child is still the same child they were before, the diagnosis didn’t change that.
—Avi’s Mom
The second one is from Jayne Dixon Weber who has been a part of the NFXF team since 2007. She’s worked with countless people and families just like you, and several years ago she wrote a letter to families with a newly diagnosed child. This is an excerpt of that letter.
I can still remember getting my son’s diagnosis, and that was over 28 years ago.
You never forget that day and where you were standing. I was devastated. All of these things ran through my mind: Having a child with a disability only happens to other people, not to me. I have all these plans for my family and for my child. We’re going to go on vacations and do all these fun things. I don’t really have time for this disability thing. I don’t really want to do this disability thing. I don’t even know what Fragile X is.
The next time I looked at my son, he changed before my eyes — he became disabled. That’s all I could see — everything he could not do or was delayed in doing. Then the guilt set in — because it came from me. That X chromosome. That. X.
Would he drive? Would he go off to college? Get married? Have children? What would his life be like? What will my life be like?
Then I heard the laugh, his laugh, the laugh that made me laugh. He didn’t know he had Fragile X. He was still the same toddler as he was yesterday. The tears came, and I picked that little guy up and said, “Why? Why me?” And then I looked at him and thought, “I don’t know if I can do this.” He continued to look at me, and I looked back at him and said, “I will do whatever I need to for you.”
Take a deep breath. You won’t be able to take care of anyone if you don’t take care of yourself. Take some time to process all that has happened and all that you have learned. You may feel grief or a sense of loss. Acknowledge those feelings. They are real, and they are normal to feel.
Now, pick up your baby or your child and give them the biggest hug. One day you will see your child as a child – you won’t see the disability. Trust me, your child really will amaze you.
—Jayne Dixon Weber
So remember, you don’t have to do anything you don’t want to do. Your most important priority right now is caring for yourself and your child. Your bond will get you both through this. For now, don’t worry about understanding all the medical and scientific terminology, because today you’re a parent.
“I would tell newly diagnosed families to not feel too overwhelmed but take things slowly. Our children will teach us a whole lot of patience, resilience, and to be happy with the small things in life. You have lovely people with huge experience to advise you, a lot of resources to help you, and your kids to teach you how to teach them.”
—FXS Parent
There’s more, but before you continue, you may want to wait before tackling everything else. If you’d like us to send you a reminder about coming back for more information when you’re ready, enter your information below (or you can use this form if you’d like to also include a message).
JUMP TO
You and Your Child
Accessing Services
Visit a Fragile X Clinic
See a Genetic Counselor
Telling Others
How to Reach Us
By Jayne Dixon Weber
Like many of you, I will always remember the day and time when I received the diagnosis of our son, Ian: Fragile X syndrome — never heard of it.

By Jayne Dixon Weber
A grandmother of a newly diagnosed grandson once called me to talk about the diagnosis. “Where is the hope?” she asked. I did not say anything to see if she would go on. “I mean, I read ‘mental retardation,’ low IQ, special education, behavior problems, delayed speech, and on and on. So, where’s the hope?”
I paused for a second. No one had ever asked me that before. I told her about the hope in my life, and I would like to share that with you.
Remember to Breathe
“Getting a diagnosis is hard. It’s really hard. There has been nothing else like it in my life and I cannot imagine there ever will be. It made me sad . . . really sad.”
—Jayne Dixon Weber
Your mind and body need breaks, and adding a few minutes of deep breathing to your daily routine can make a difference. What you’re going through right now is hard . . . and confusing and overwhelming . . . and you’re perfectly normal if you’re also feeling angry, bitter, guilty, afraid — of the knowns and the unknowns — and yes, sad.
If you’re feeling anxious or overwhelmed right now, take a slow, deep breath . . . in through your nose, focusing on the incoming air filling your belly . . . then a slow exhale out through your nose.
On the next breath, place one hand on your belly and one on your chest. Take another slow deep breath in through your nose, this time focusing on the feel of your belly rising, then your chest (just a little), and exhale out your nose, emptying your chest first, then your belly. Repeat three times.
Also watch our webinar from psychologist and research scientist Anne Wheeler: Using Mindfulness and Acceptance Techniques to Reduce Stress and Improve Coping↗.
Make Self-Care a Priority
We humans tend to ignore self-care during a crisis, but focusing on your physical and mental health right now can lessen your stress and anxiety in the long run. We can’t stress this enough.
Part of your job of caring for your child is caring for yourself. Think of like when you’re a passenger on an airplane, and the flight attendant instructs you to put the oxygen mask on yourself before you put one on your child.
If you’re not there, who will put their mask on?
The emotions you’re going through right now are intense and new. How long they last will vary, and rather than ignoring them, try to acknowledge them. We promise, the intensity will lessen.
Signs of Caregiver Stress
- Feeling overwhelmed
- Feeling sad
- Constant worrying
- Feeling tired most of the time
- Getting too much sleep
- Not getting enough sleep
- Gaining weight
- Losing weight
- Easily angered or irritated
- Loss of interest in things you used to enjoy
- Frequent headaches or other physical pain
- Abusing alcohol and other drugs
Tips for Managing Stress
- Accept help
- Focus on what you can provide to your child (no one’s perfect)
- Set realistic goals and break them down into smaller tasks
- Connect with others in your social circle, support groups, and resources to streamline some of your responsibilities
- Set healthy goals for yourself
- See a doctor or therapist
Read more from the Mayo Clinic on “Caregiver stress: Tips for taking care of yourself”↗
Find a Therapist↗ is a tool from Psychology Today. If your emotions continue to feel overwhelming, this will help you find a local (or by teletherapy) therapist, psychiatrist, or treatment center near you.
When Your Doctor Says “I Have Bad News”↗ from Jessie Gruman, who has interviewed hundreds of people who have dealt with serious diagnoses, and she has survived four cancer scares herself. She asserts that even though a scary diagnosis can turn your world upside down, there are practical strategies you can use to take the best next steps and bring balance back to your life.
Gaiam’s YouTube channel↗ offers an amazing number of videos and playlists in categories like yoga, meditation, fitness, and discovery. No matter how much time you have, you can find one that fits your schedule.
Yoga With Adriene↗ offers a 30-day yoga course on YouTube. Day one is learning breathing techniques and moves into poses, stretches, and cool downs.
How to Start and Write a Journal↗ breaks down the steps you can take to keep your thoughts organized and your mind clear through regular journaling.
10 Podcasts for Anxiety↗ provides a curated list of podcasts on dealing with anxiety, including tools, tips, and relaxation techniques.
How to Use Drawing as a Coping Tool for Anxiety↗ lays out the benefits of drawing, plus easy exercises and tips and tricks to get you started.
Learning to Observe and Accept Your Emotions↗ from Verywell Mind.
Reach Out to the National Fragile X Foundation: See the form on this page, or:
- Email: treatment@fragilex.org
- Phone: (800) 688-8765
Hug Your Child
At the end of the day remember that your child is still the same wonderful, unique child you’ve loved since they were born. The diagnosis didn’t change that.
What will change is you’ll learn about things you never knew existed. You’ll become a more understanding person. You’ll develop a love for your child that will amaze you. Your child learns differently than you do, but they can and will learn — with your help.
Two Letters
We have two letters to share with you.
The first one is from Avi’s mom. We often ask parents for their advice for newly diagnosed parents, and she wrote this just seven months after Avi’s diagnosis. This is Avi.

My advice for newly diagnosed families is to first allow yourself permission to grieve; to mourn the life you had imagined for your child, the life you had imagined for your family, the hopes and dreams that you had envisioned.
Understand that it is okay to feel whatever you’re feeling; to be sad, angry, worried, lost, and confused.
Then, begin reaching out to other families who understand what you’re going through. Join a Community Support Network↗ near you.
Be leery of the internet. While it can be a tool of knowledge, it can also be a tool of misinformation and negativity.
Know that support from friends and family is important, but, no matter how they try, they may never understand or “get it.”
The grief comes and goes in waves. We only found out 7 months ago, and I am still constantly cycling between anger, hopelessness, sadness, empowerment, strength, courage, hope, and then anger again.
Most days though are days of strength and courage because there’s no other choice. My sweet boy needs a strong mama who can spread awareness, advocate for his needs, be a voice for him since he hasn’t quite found his yet, roll cars and trucks back and forth for what seems like hours, and give unlimited hugs and kisses.
A diagnosis can drive treatment and intervention, but at the end of the day remember that your child is still the same child they were before, the diagnosis didn’t change that.
—Avi’s Mom
The second one is from Jayne Dixon Weber who has been a part of the NFXF team since 2007. She’s worked with countless people and families just like you, and several years ago she wrote a letter to families with a newly diagnosed child. This is an excerpt of that letter.
I can still remember getting my son’s diagnosis, and that was over 28 years ago.
You never forget that day and where you were standing. I was devastated. All of these things ran through my mind: Having a child with a disability only happens to other people, not to me. I have all these plans for my family and for my child. We’re going to go on vacations and do all these fun things. I don’t really have time for this disability thing. I don’t really want to do this disability thing. I don’t even know what Fragile X is.
The next time I looked at my son, he changed before my eyes — he became disabled. That’s all I could see — everything he could not do or was delayed in doing. Then the guilt set in — because it came from me. That X chromosome. That. X.
Would he drive? Would he go off to college? Get married? Have children? What would his life be like? What will my life be like?
Then I heard the laugh, his laugh, the laugh that made me laugh. He didn’t know he had Fragile X. He was still the same toddler as he was yesterday. The tears came, and I picked that little guy up and said, “Why? Why me?” And then I looked at him and thought, “I don’t know if I can do this.” He continued to look at me, and I looked back at him and said, “I will do whatever I need to for you.”
Take a deep breath. You won’t be able to take care of anyone if you don’t take care of yourself. Take some time to process all that has happened and all that you have learned. You may feel grief or a sense of loss. Acknowledge those feelings. They are real, and they are normal to feel.
Now, pick up your baby or your child and give them the biggest hug. One day you will see your child as a child – you won’t see the disability. Trust me, your child really will amaze you.
—Jayne Dixon Weber
So remember, you don’t have to do anything you don’t want to do. Your most important priority right now is caring for yourself and your child. Your bond will get you both through this. For now, don’t worry about understanding all the medical and scientific terminology, because today you’re a parent.
“I would tell newly diagnosed families to not feel too overwhelmed but take things slowly. Our children will teach us a whole lot of patience, resilience, and to be happy with the small things in life. You have lovely people with huge experience to advise you, a lot of resources to help you, and your kids to teach you how to teach them.”
—FXS Parent
There’s more, but before you continue, you may want to wait before tackling everything else. If you’d like us to send you a reminder about coming back for more information when you’re ready, enter your information below (or you can use this form if you’d like to also include a message).
JUMP TO
You and Your Child
Accessing Services
Visit a Fragile X Clinic
See a Genetic Counselor
Telling Others
How to Reach Us
By Jayne Dixon Weber
Like many of you, I will always remember the day and time when I received the diagnosis of our son, Ian: Fragile X syndrome — never heard of it.

By Jayne Dixon Weber
A grandmother of a newly diagnosed grandson once called me to talk about the diagnosis. “Where is the hope?” she asked. I did not say anything to see if she would go on. “I mean, I read ‘mental retardation,’ low IQ, special education, behavior problems, delayed speech, and on and on. So, where’s the hope?”
I paused for a second. No one had ever asked me that before. I told her about the hope in my life, and I would like to share that with you.
Breathing Exercises
Breathing exercises have been proven to help with stress and anxiety symptoms. If you’re feeling like you need relief right now, try this:
- Stand up (or sit up straight and tall).
- Pull your shoulders back.
- Plant your feet evenly and widely apart.
- Open your chest.
- Breathe deeply.
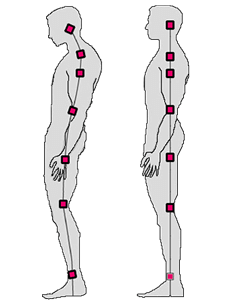
What This Does: Deep breathing while in this position tells your body you’re not in danger at this moment. You should feel less helpless and a little more in control.
For this and other relaxation techniques, see from Inc.:
9 Ways to Get Rid of Anxiety in 5 Minutes or Less↗
Also see from Healthline:
8 Breathing Exercises to Try When You Feel Anxious↗
Breathing Exercises
Breathing exercises have been proven to help with stress and anxiety symptoms. If you’re feeling like you need relief right now, try this:
- Stand up (or sit up straight and tall).
- Pull your shoulders back.
- Plant your feet evenly and widely apart.
- Open your chest.
- Breathe deeply.
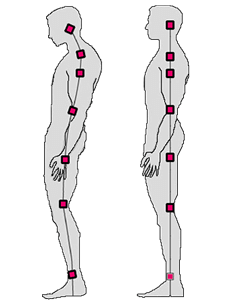
What This Does: Deep breathing while in this position tells your body you’re not in danger at this moment. You should feel less helpless and a little more in control.
For this and other relaxation techniques, see from Inc.:
9 Ways to Get Rid of Anxiety in 5 Minutes or Less↗
Also see from Healthline:
8 Breathing Exercises to Try When You Feel Anxious↗
2. Everything Else
When You’re Ready
Here we address other steps you may need to take, depending on your situation. And remember, you can always contact us for advice and resources specific to you and your child.
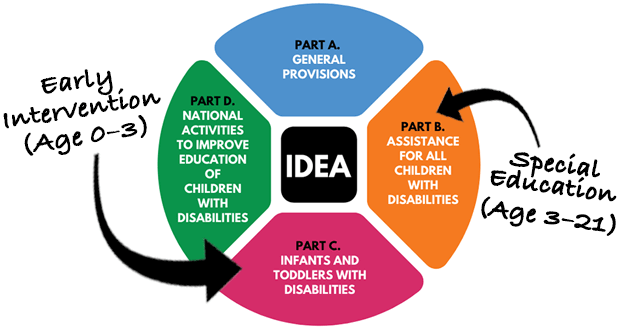
Accessing Services
For families in the U.S., your child with Fragile X syndrome is eligible for services under the federal special education law IDEA, the Individuals with Disabilities Education Act, which ensures access to early intervention (ages 0–3) and later (ages 3–21) “appropriate” public education for eligible children with disabilities. Services are free (or at reduced cost), and available in every U.S. state or territory.
It’s important to know that while every state has services under IDEA, each state has their own system for coordinating these services, including evaluation and eligibility requirements. Specific instructions are provided below.
Overview
Children whose development is affected by Fragile X syndrome are eligible for special education services through the federal law called IDEA, or Individuals with Disabilities Education Act:
- Part C: Birth to 36 months
- Part B: 36 months to 21 years
IDEA requires a multidisciplinary evaluation to determine if the child qualifies for special education services. This means that professionals from a variety of fields (medicine, psychology, occupational therapy, etc.) and the parents of the child collaborate to assess the child’s strengths and needs and determine appropriate educational services.
Every child eligible has either an individualized family service plan (or IFSP, for children birth to 36 months), or an individualized education program (or IEP, for children age 36 months to 21 years). Both of these programs specify the details of a child’s educational plan.
Intervention varies and is based on the child’s individual needs. Areas that may be addressed include: speech and language, cognition, behavior, sensory-motor, and academics. Settings range from home-based programs for infants to a variety of school-based classrooms for older children.
Part C: Infants and Toddlers with Disabilities
The human brain is most adaptable in the first three years. This is when the brain is growing at a rapid rate and, amazingly, it will double in size in the first year alone. These programs can have a profound impact on your child’s ability to learn new skills throughout their lifetime.
Part C Summary
- For eligible infants and toddlers (age 0–36 months) and their families.
- Families work with an assigned service coordinator↗during any multidisciplinary evaluations or assessments.
- Before early intervention services are put into place, a written plan detailing the early intervention services — the individualized family service plan, or IFSP — must be created and reviewed every six months (or more often if needed). You, as the parent or caregiver, will be a part of the team developing the IFSP.
- A transition plan must be developed as part of the IFSP (no later than 90 days prior to the child’s third birthday) to ensure a smooth transition into Part B services.
How to Access Your Part C Coordinator*
- Find your Part C coordinator by state↗
- Click on your state name.
- Call, email, fax, or write to your state contact.
- Set up an appointment to meet with your coordinator.
*Your doctor can also refer you, but their referral is not required.
Early Intervention for Infants and Toddlers with Fragile X Syndrome↗ How it works, step by step.
Print the IDEA Part C statute↗
Wrightslaw↗ This is our go-to site for anything related to special education law and advocacy.
Learn the Signs↗ from the CDC.
Overview of Early Intervention↗ from the Center for Parent Information and Resources
Early Intervention Program for Infants and Toddlers with Disabilities↗ from Benefits.gov
Download the model IFSP form↗ published by the U.S. Department of Education.
State Examples of IFSP Forms and Guidance↗ from the Early Childhood Technical Assistance Center.
Newborn, Carrier, and Early Childhood Screening Recommendations for Fragile X↗ from our treatment and intervention recommendations.
Part B: Assistance for All Children With Disabilities
Part B of IDEA governs how special education and related services are provided to school-aged children (ages 3–22) with disabilities.
Part B Summary
- For eligible children age 3–21 years, and early childhood special education (or ECSE) applies to ages 3–5 years.
- Families work with preschool programs within their local school district.
- Before early childhood special education services can be put into place, a written plan — this time called an individualized education plan, or IEP — must be created. IEPs are similar to IFSPs, but focus more on the child than the family as a whole.
How to Access Your Part B Coordinator*
- Locate your Part B coordinators by state↗
- Click on your state name.
- Call, email, fax, or write to your state contact.
- Set up an appointment to meet with your coordinator.
*Your local school district or doctor can also refer you, but their referral is not required.
Preparing for Your Child’s Individual Education Program (IEP)
From the Center for Parent Information and Resources:
Print the IDEA Part B statute↗
Wrightslaw↗ This is our go-to site for anything related to special education law and advocacy.
JUMP TO
You and Your Child
Accessing Services
Visit a Fragile X Clinic
See a Genetic Counselor
Telling Others
How to Reach Us

Your guide to the early intervention process, including the multidisciplinary evaluation and assessment, parent preparation, the individualized family service plan (IFSP), examples of early intervention services you may receive, examples of goals for infants and toddlers, where and how services may be provided, family rights, and the transition plan when moving to Part B.
Accessing Services
For families in the U.S., your child with Fragile X syndrome is eligible for services under the federal special education law IDEA, the Individuals with Disabilities Education Act, which ensures access to early intervention (ages 0–3) and later (ages 3–21) “appropriate” public education for eligible children with disabilities. Services are free (or at reduced cost), and available in every U.S. state or territory.
It’s important to know that while every state has services under IDEA, each state has their own system for coordinating these services, including evaluation and eligibility requirements. Specific instructions are provided below.
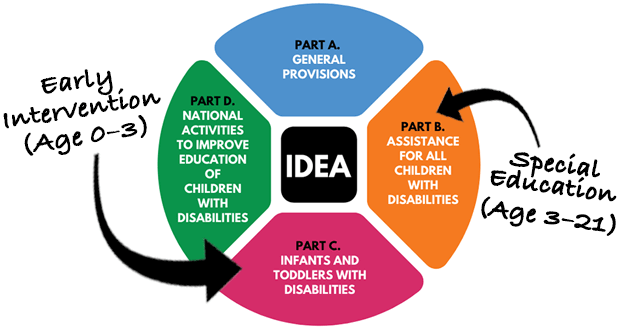
Overview
Children whose development is affected by Fragile X syndrome are eligible for special education services through the federal law called IDEA, or Individuals with Disabilities Education Act:
- Part C: Birth to 36 months
- Part B: 36 months to 21 years
IDEA requires a multidisciplinary evaluation to determine if the child qualifies for special education services. This means that professionals from a variety of fields (medicine, psychology, occupational therapy, etc.) and the parents of the child collaborate to assess the child’s strengths and needs and determine appropriate educational services.
Every child eligible has either an individualized family service plan (or IFSP, for children birth to 36 months), or an individualized education program (or IEP, for children age 36 months to 21 years). Both of these programs specify the details of a child’s educational plan.
Intervention varies and is based on the child’s individual needs. Areas that may be addressed include: speech and language, cognition, behavior, sensory-motor, and academics. Settings range from home-based programs for infants to a variety of school-based classrooms for older children.
Part C: Infants and Toddlers with Disabilities
The human brain is most adaptable in the first three years. This is when the brain is growing at a rapid rate and, amazingly, it will double in size in the first year alone. These programs can have a profound impact on your child’s ability to learn new skills throughout their lifetime.
Part C Summary
- For eligible infants and toddlers (age 0–36 months) and their families.
- Families work with an assigned service coordinator↗during any multidisciplinary evaluations or assessments.
- Before early intervention services are put into place, a written plan detailing the early intervention services — the individualized family service plan, or IFSP — must be created and reviewed every six months (or more often if needed). You, as the parent or caregiver, will be a part of the team developing the IFSP.
- A transition plan must be developed as part of the IFSP (no later than 90 days prior to the child’s third birthday) to ensure a smooth transition into Part B services.
How to Access Your Part C Coordinator*
- Find your Part C coordinator by state↗
- Click on your state name.
- Call, email, fax, or write to your state contact.
- Set up an appointment to meet with your coordinator.
*Your doctor can also refer you, but their referral is not required.
Early Intervention for Infants and Toddlers with Fragile X Syndrome↗ How it works, step by step.
Print the IDEA Part C statute↗
Wrightslaw↗ This is our go-to site for anything related to special education law and advocacy.
Learn the Signs↗ from the CDC.
Overview of Early Intervention↗ from the Center for Parent Information and Resources
Early Intervention Program for Infants and Toddlers with Disabilities↗ from Benefits.gov
Download the model IFSP form↗ published by the U.S. Department of Education.
State Examples of IFSP Forms and Guidance↗ from the Early Childhood Technical Assistance Center.
Newborn, Carrier, and Early Childhood Screening Recommendations for Fragile X↗ from our treatment and intervention recommendations.
Part B: Assistance for All Children With Disabilities
Part B of IDEA governs how special education and related services are provided to school-aged children (ages 3–22) with disabilities.
Part B Summary
- For eligible children age 3–21 years, and early childhood special education (or ECSE) applies to ages 3–5 years.
- Families work with preschool programs within their local school district.
- Before early childhood special education services can be put into place, a written plan — this time called an individualized education plan, or IEP — must be created. IEPs are similar to IFSPs, but focus more on the child than the family as a whole.
How to Access Your Part B Coordinator*
- Locate your Part B coordinators by state↗
- Click on your state name.
- Call, email, fax, or write to your state contact.
- Set up an appointment to meet with your coordinator.
*Your local school district or doctor can also refer you, but their referral is not required.
Preparing for Your Child’s Individual Education Program (IEP)
From the Center for Parent Information and Resources:
Print the IDEA Part B statute↗
Wrightslaw↗ This is our go-to site for anything related to special education law and advocacy.
JUMP TO
You and Your Child
Accessing Services
Visit a Fragile X Clinic
See a Genetic Counselor
Telling Others
How to Reach Us

Your guide to the early intervention process, including the multidisciplinary evaluation and assessment, parent preparation, the individualized family service plan (IFSP), examples of early intervention services you may receive, examples of goals for infants and toddlers, where and how services may be provided, family rights, and the transition plan when moving to Part B.
Fragile X 101: A guide for the newly-diagnosed and those already living with Fragile X
Receiving a diagnosis of a Fragile X disorder presents a distinct challenge for individuals and their families. Our guide is written for you to learn the basics and to continue to use as a reference.
Print or save it to your computer to share with others who may ask you for more information, including questions about genetics and inheritance, characteristics, treatment, research, and potential health issues.
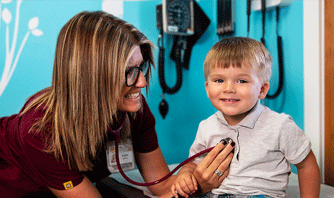
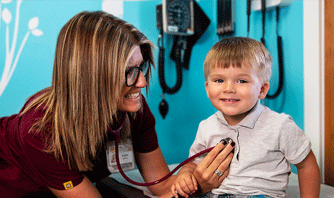
Visit a Fragile X Clinic
If you haven’t already connected with a Fragile X clinic, we encourage you to do so now.
What’s a Fragile X Clinic?
Fragile X clinics are part of the Fragile X Clinical and Research Consortium, which was created by us — the National Fragile X Foundation — in response to the growing needs of families whose members have one of the Fragile X-associated disorders. The consortium is composed of 30-plus clinics across the U.S., each of which has expertise in Fragile X.
- Fragile X clinics know and understand the difficulties families face when searching for the right services or local providers who have heard of Fragile X.
- Fragile X clinics can work with your local providers to help manage any ongoing or acute issues.
- Fragile X clinics may know of new information that has not made it to the general public yet.
What to Expect
Once you locate a clinic (see our map below), you’ll reach out to the clinic coordinator who will guide you through the process, including working with you to complete intake forms and gather relevant records, which may include:
Your Child’s Records
- Fragile X test lab results
- Current or past medications
- Other relevant medical records
The following may also be requested, depending on the child’s age:
- Psychological, cognitive, or ophthalmological evaluation records
- School records
Your Family History
Clinic intake forms typically include questions related to your family history with Fragile X. Provide what you have and don’t worry about the rest at this point. The important thing here is connecting with a Fragile X clinic.
If you have previously met with a genetic counselor , you may have worked with them to gather this information — but at this early stage in your journey, you may not have access to the information, or it may not exist. But don’t worry, the clinic will walk you through all of this. Here’s some of what they may ask regarding your extended family, both living and deceased:
- Known diagnoses: For any individuals with developmental delays, behavioral disorders, neurological disorders (including late onset Fragile X-associated tremor/ataxia syndrome or primary ovarian insufficiency), and fertility issues.
- Photos: Of family members who have or are suspected of having Fragile X syndrome.
- Medical records: Including genetic tests; pediatric, medical, or psychiatric records; or psychological, speech, and occupational therapy evaluations.
- Educational records: From school therapists or teachers.
- Baby books, scrapbooks, and journals: These sources may help reveal ages of developmental milestones, illnesses, medications (including any reactions), therapeutic interventions, and more.
Once your forms and records are reviewed, they’ll then work with you to schedule the appropriate appointment or appointments. Keep in mind that initial, comprehensive assessments may take more than one day or visit.
To learn more about what to expect from your first visit, see from our Fragile X Info Series: Your In-Person Visit to a Fragile X Clinic↗
Find Your Fragile X Clinic ↓
See our map below, or visit our Fragile X Clinics page↗.
JUMP TO
You and Your Child
Accessing Services
Visit a Fragile X Clinic
See a Genetic Counselor
Telling Others
How to Reach Us

You will be happier with your visit and get more out of it if you take an active role in the process ahead of time. We have lists for everything you’ll need.
Why a Fragile X clinic might be exactly what you were looking for.
 We’ve created several downloadable/printable resource sheets for different topics (see all↗), including this one to prepare for an in-person visit to a Fragile X clinic.
We’ve created several downloadable/printable resource sheets for different topics (see all↗), including this one to prepare for an in-person visit to a Fragile X clinic.
Visit a Fragile X Clinic
If you haven’t already connected with a Fragile X clinic, we encourage you to do so now.
What’s a Fragile X Clinic?
Fragile X clinics are part of the Fragile X Clinical and Research Consortium, which was created by us — the National Fragile X Foundation — in response to the growing needs of families whose members have one of the Fragile X-associated disorders. The consortium is composed of 30-plus clinics across the U.S., each of which has expertise in Fragile X.
- Fragile X clinics know and understand the difficulties families face when searching for the right services or local providers who have heard of Fragile X.
- Fragile X clinics can work with your local providers to help manage any ongoing or acute issues.
- Fragile X clinics may know of new information that has not made it to the general public yet.
What to Expect
Once you locate a clinic (see our map below), you’ll reach out to the clinic coordinator who will guide you through the process, including working with you to complete intake forms and gather relevant records, which may include:
Your Child’s Records
- Fragile X test lab results
- Current or past medications
- Other relevant medical records
The following may also be requested, depending on the child’s age:
- Psychological, cognitive, or ophthalmological evaluation records
- School records
Your Family History
Clinic intake forms typically include questions related to your family history with Fragile X. Provide what you have and don’t worry about the rest at this point. The important thing here is connecting with a Fragile X clinic.
If you have previously met with a genetic counselor , you may have worked with them to gather this information — but at this early stage in your journey, you may not have access to the information, or it may not exist. But don’t worry, the clinic will walk you through all of this. Here’s some of what they may ask regarding your extended family, both living and deceased:
- Known diagnoses: For any individuals with developmental delays, behavioral disorders, neurological disorders (including late onset Fragile X-associated tremor/ataxia syndrome or primary ovarian insufficiency), and fertility issues.
- Photos: Of family members who have or are suspected of having Fragile X syndrome.
- Medical records: Including genetic tests; pediatric, medical, or psychiatric records; or psychological, speech, and occupational therapy evaluations.
- Educational records: From school therapists or teachers.
- Baby books, scrapbooks, and journals: These sources may help reveal ages of developmental milestones, illnesses, medications (including any reactions), therapeutic interventions, and more.
Once your forms and records are reviewed, they’ll then work with you to schedule the appropriate appointment or appointments. Keep in mind that initial, comprehensive assessments may take more than one day or visit.
To learn more about what to expect from your first visit, see from our Fragile X Info Series: Your In-Person Visit to a Fragile X Clinic↗
Find Your Fragile X Clinic
See our map below, or visit our Fragile X Clinics page↗.
JUMP TO
You and Your Child
Accessing Services
Visit a Fragile X Clinic
See a Genetic Counselor
Telling Others
How to Reach Us

You will be happier with your visit and get more out of it if you take an active role in the process ahead of time. We have lists for everything you’ll need.
Why a Fragile X clinic might be exactly what you were looking for.
 We’ve created several downloadable and printable resource sheets for different topics (see all↗), including this one to prepare for an in-person visit to a Fragile X clinic.
We’ve created several downloadable and printable resource sheets for different topics (see all↗), including this one to prepare for an in-person visit to a Fragile X clinic.
See a Genetic Counselor
Due to the complexity of Fragile X, a genetic counselor is a must.
A genetic counselor is a trained, master-level health care professional who will work side-by-side with you to educate, counsel, and guide you through this early part of your journey. This is your chance to ask as many questions as you need to — and get answers from an expert.
TIP: Keep a notepad (either a real one, or a phone app) with you throughout the day so you can write down questions as they occur to you.
What else does a genetic counselor do? In addition to answering all your questions, your counselor can make referrals to other providers for therapies or medical evaluations (for your child), or family counseling or emotional support (for you and your family).
They’ll also guide you through understanding:
- Your child’s diagnosis. (For older children, also see: Making Sense of Multiple Diagnoses.)
- The facts and options for managing your child’s condition.
- Symptoms of other Fragile X-associated disorders, including infertility, early menopause, and/or adult onset neurological or movement disorders.
- How to talk to your other children (if any), including helping them understand the condition.
- Reproductive issues and options for family planning.
- Fragile X inheritance patterns (i.e., how it gets passed down).
- Whether you and/or your child’s other parent is a carrier (and what that means).
- The pros and cons of telling your relatives.
How to Find a Genetic Counselor
We recommend making an appointment at your nearest Fragile X clinic. Fragile X clinics provide genetic counseling and medical services (including medication evaluations and consultations) supervised by a physician and supported by the latest medical, educational, and research knowledge available. Multidisciplinary services, such as occupational, speech, language, and behavioral therapies, are also available either at the clinic or by referral.
If you’re concerned about your ability to visit a Fragile X clinic for financial reasons, call them anyway and ask about the Fly With Me Fund.
Ask your doctor or other health
professional for a referral
to a local genetic counselor.
From the National Society of Genetic Counselors:
Find a Genetic Counselor↗
Contact us:
Email↗
(800) 688-8765↗
Genetics & Inheritance
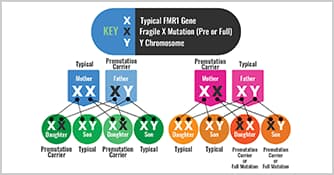
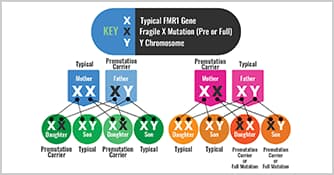
A genetics specialist can help you learn and understand how Fragile X-associated disorders are passed down in families through expansions of the FMR1 gene. Even for genetics professionals, FMR1 inheritance is complex and confusing, so it’s no surprise that families often have questions. To better understand this, your genetic counselor will also help orient you to the various terms and how it all works, and we also have resources for learning how the FMR1 gene causes Fragile X syndrome, including:
- Our pages on genetics and inheritance
- How Fragile X Syndrome is Inherited↗ from the CDC
- Inheritance Patterns for Single Gene Disorders↗ from the Genetic Science Learning Center.
Watch This ↓
We recently presented a webinar from Brenda Finucane, a licensed genetic counselor. Watch The Genetics of Fragile X-Associated Disorders — available below.
JUMP TO
You and Your Child
Accessing Services
Visit a Fragile X Clinic
See a Genetic Counselor
Telling Others
How to Reach Us

Learn more about who should seek out a genetic counselor? What does a genetic counselor do? And what to expect.
Our consensus documents (professional recommendations) can be a bit dry for us laymen, but they’re written by the top experts in the field and go through an editing and review process with our Fragile X Clinical and Research Consortium members and its Clinical Practices Committee.
See a Genetic Counselor
Due to the complexity of Fragile X, a genetic counselor is a must.
A genetic counselor is a trained, master-level health care professional who will work side-by-side with you to educate, counsel, and guide you through this early part of your journey. This is your chance to ask as many questions as you need to — and get answers from an expert.
TIP: Keep a notepad (either a real one, or a phone app) with you throughout the day so you can write down questions as they occur to you.
What else does a genetic counselor do? In addition to answering all your questions, your counselor can make referrals to other providers for therapies or medical evaluations (for your child), or family counseling or emotional support (for you and your family).
They’ll also guide you through understanding:
- Your child’s diagnosis. (For older children, also see: Making Sense of Multiple Diagnoses.)
- The facts and options for managing your child’s condition.
- Symptoms of other Fragile X-associated disorders, including infertility, early menopause, and/or adult onset neurological or movement disorders.
- How to talk to your other children (if any), including helping them understand the condition.
- Reproductive issues and options for family planning.
- Fragile X inheritance patterns (i.e., how it gets passed down).
- Whether you and/or your child’s other parent is a carrier (and what that means).
- The pros and cons of telling your relatives.
How to Find a Genetic Counselor
We recommend making an appointment at your nearest Fragile X clinic. Fragile X clinics provide genetic counseling and medical services (including medication evaluations and consultations) supervised by a physician and supported by the latest medical, educational, and research knowledge available. Multidisciplinary services, such as occupational, speech, language, and behavioral therapies, are also available either at the clinic or by referral.
If you’re concerned about your ability to visit a Fragile X clinic for financial reasons, call them anyway and ask about the Fly With Me Fund.
Ask your doctor or other health
professional for a referral
to a local genetic counselor.
From the National Society of Genetic Counselors:
Find a Genetic Counselor↗
Contact us:
Email↗
(800) 688-8765↗
Genetics & Inheritance
A genetics specialist can help you learn and understand how Fragile X-associated disorders are passed down in families through expansions of the FMR1 gene. Even for genetics professionals, FMR1 inheritance is complex and confusing, so it’s no surprise that families often have questions. To better understand this, your genetic counselor will also help orient you to the various terms and how it all works, and we also have resources for learning how the FMR1 gene causes Fragile X syndrome, including:
- Our pages on genetics and inheritance
- How Fragile X Syndrome is Inherited↗ from the CDC
- Inheritance Patterns for Single Gene Disorders↗ from the Genetic Science Learning Center.
JUMP TO
You and Your Child
Accessing Services
Visit a Fragile X Clinic
See a Genetic Counselor
Telling Others
How to Reach Us

Learn more about who should seek out a genetic counselor? What does a genetic counselor do? And what to expect.
Our consensus documents (professional recommendations) can be a bit dry for us laymen, but they’re written by the top experts in the field and go through an editing and review process with our Fragile X Clinical and Research Consortium members and its Clinical Practices Committee.
Watch This ↓
We recently presented a webinar from Brenda Finucane, a licensed genetic counselor. Watch The Genetics of Fragile X-Associated Disorders — available below.
Brenda Finucane, MS, LGC, is a licensed genetic counselor and professor at Geisinger’s Autism & Developmental Medicine Institute↗. She is currently a genetic counseling consultant for the NFXF. Also see: Google Scholar Profile↗.
The Genetics of Fragile X-Associated Disorders
With Brenda Finucane
Brenda Finucane helps us understand the genetics of Fragile X syndrome, Fragile X-associated tremor/ataxia syndrome, and Fragile X-associated primary overian insufficiency, also known as FXS (fax-ess), FXTAS (fax-tass), and FXPOI (fax-poy).
The Genetics of Fragile X-Associated Disorders
With Brenda Finucane
Brenda Finucane helps us understand the genetics of Fragile X syndrome, Fragile X-associated tremor/ataxia syndrome, and Fragile X-associated primary overian insufficiency, also known as FXS (fax-ess), FXTAS (fax-tass), and FXPOI (fax-poy).
Brenda Finucane, MS, LGC, is a licensed genetic counselor and professor at Geisinger’s Autism & Developmental Medicine Institute↗. She is currently a genetic counseling consultant for the NFXF. Also see: Google Scholar Profile↗.
Telling Others
Who are “others”? If you have other children, you’ll need to help them understand what’s going on, and you’ll need to tell your extended family.
Telling Your “Typical” Children
If you’ve visited a genetic counselor, they’re specially trained to help explain complex genetic information in a way that is understandable to families, and help you with how to approach the subject and any recommended ongoing conversations.
But, if this falls solely on you (or in partnership with a spouse or other partner), we’ve found that, fortunately, many of the same strategies for the “sex talk” apply equally to the Fragile X talk ↗. For children too young to understand this approach, creating an open dialog within the family is a good first step.
Telling Relatives
When informing relatives about Fragile X syndrome — some of whom may react with anger, guilt, blame, disbelief, or indifference — we again recommend working with your genetic counselor to develop a strategy for informing relatives and how to best approach the subject of diagnostic or carrier testing.
Difficult ethical situations can develop when a family member refuses to share information about Fragile X syndrome to at-risk relatives. In addition to identifying at-risk relatives, your counselor will work with you to inform family members, and to coordinate testing throughout the family.
Telling relatives about their risk of being a Fragile X carrier should happen sooner rather than later, but what if the earliest appointment to see a genetic counselor isn’t for another month, or longer? Do you wait that long?
Depending on your extended family situation, you may be able to wait. But if not (if you’re not sure, ask us ), another option is sending a letter (we’ve provided a template for you below) that summarizes the situation and refers them to someone other than yourself for questions. We’ve found this to be the most stress-free solution, especially if you’re not comfortable talking to relatives. Ideally you would refer them to your genetic counselor, but if you haven’t met with one yet, you can refer them to us, which we’ve included in the letter.
Dear Family
The letter is in Word format and may be altered it to suit your situation. We hope this helps you deal with the delicate nature of explaining this complex information to family members, some of whom you may not even know. Keep in mind:
- It is not your responsibility to provide genetic counseling or to ensure your family members pursue testing.
- The letter in its original form is anonymous and does not refer to who the family member is that’s been diagnosed.
- You can sign you name in the letter, or it can be sent anonymously.
- If you need your relatives to help you locate other family members, include that information in the letter along with copies of an appropriate fact sheet that they can share with others — see our Info Series fact sheets and our Fragile X 101 ebook .
Below is the contents of the letter, which is available as a Word document:
To Whom It May Concern:
A member of your family has been identified as either having a condition called Fragile X syndrome (FXS) or being a carrier of a genetic change that could cause a Fragile X disorder (FXD). This means that other family members may also be carriers of this gene change and/or be at risk to have children with FXS. This letter has been sent to you to summarize information regarding the genetics of FXDs and Fragile X syndrome.
Fragile X syndrome is the most common form of inherited intellectual disabilities. It can occur in both males and females, though females often have milder features than males. Affected individuals can have intellectual disabilities, learning and behavioral disorders and/or autism. Other characteristics include repetitive speech, hyperactivity, and poor eye contact. Physical characteristics include large ears, flexible joints and a long face.
Fragile X is caused by a genetic change (mutation) in a gene called the FMR1 gene, which is on the X chromosome.
The Fragile X gene exists in a number of forms. An individual may carry a normal size gene, a “premutation” size gene or a “full mutation” size gene. Both males and females can inherit this gene in either the premutation or full mutation form. Often individuals with a premutation are referred to as “premutation carriers.”
Individuals with FXS have a full mutation gene. Individuals with a premutation are usually not affected with FXS but are at risk to have children or grandchildren with a full mutation.
Females have two X chromosomes. Women who have inherited the Fragile X gene in either the full or premutation form are at risk to have a child with FXS.
Males have one X chromosome inherited from their mother and one Y chromosome inherited from their father. Males who have inherited a full mutation from their mother will have FXS. Males who inherit a premutation will pass it on to all of their daughters and to none of their sons. In other words, all the daughters of male carriers will be carriers themselves.
Individuals who are premutation carriers are usually not affected, but they are susceptible to two other conditions:
- Fragile X-associated primary ovarian insufficiency (abbreviated FXPOI, pronounced “fax-poy”)—Seen in some women with the premutation, it results in early menopause and/or reduced fertility.
- Fragile X-associated tremor/ataxia syndrome (abbreviated FXTAS, pronounced “fax-tas”)—A late onset (over age 50) neurological condition, sometimes initially diagnosed as Parkinson’s disease, that is more common in males than females.
Therefore, even if you are not in your childbearing years, the possibility of being a Fragile X gene carrier has implications for your health, your children’s or your grandchildren’s health.
A DNA test for FXDs, called the “FMR1 DNA test,” has been available since 1991. This test is extremely reliable in detecting the premutation or full mutation of Fragile X. Since a member of your family has been identified as carrying this gene change, you and your children (if you have any), may also carry this changed gene. It is therefore recommended that you and/or your children contact a genetic counselor to discuss your family history and the advisability of genetic testing. Your physician or other health care provider can order this testing on your behalf.
Your options should you wish to discuss the contents of this letter:
- You can locate a genetic counselor in your geographical area at www.nsgc.org.
- You can find additional information on the NFXF website by reviewing the section for “Newly Diagnosed” under the Living With Fragile X heading on the main menu at fragilex.org
We hope this information is of help to you. Please feel free to use any or all of the resources described above and should you have any further questions, you can contact the National Fragile X Foundation by phone at (800) 688-8765 or by email at treatment@fragilex.org.
Sincerely,
XXXXXXXX
JUMP TO
You and Your Child
Accessing Services
Visit a Fragile X Clinic
See a Genetic Counselor
Telling Others
How to Reach Us

Many families struggle with deciding when the “right” time is and what to say. Here are some strategies to help in having a conversation with your daughter about her Fragile X syndrome diagnosis.

Families do best when there is open and honest communication about Fragile X. Here’s our tips on how and when to start the conversation.
Telling Others
Who are “others”? If you have other children, you’ll need to help them understand what’s going on, and you’ll need to tell your extended family.
Telling Your “Typical” Children
If you’ve visited a genetic counselor, they’re specially trained to help explain complex genetic information in a way that is understandable to families, and help you with how to approach the subject and any recommended ongoing conversations.
But, if this falls solely on you (or in partnership with a spouse or other partner), we’ve found that, fortunately, many of the same strategies for the “sex talk” apply equally to the Fragile X talk ↗. For children too young to understand this approach, creating an open dialog within the family is a good first step.
Telling Relatives
When informing relatives about Fragile X syndrome — some of whom may react with anger, guilt, blame, disbelief, or indifference — we again recommend working with your genetic counselor to develop a strategy for informing relatives and how to best approach the subject of diagnostic or carrier testing.
Difficult ethical situations can develop when a family member refuses to share information about Fragile X syndrome to at-risk relatives. In addition to identifying at-risk relatives, your counselor will work with you to inform family members, and to coordinate testing throughout the family.
Telling relatives about their risk of being a Fragile X carrier should happen sooner rather than later, but what if the earliest appointment to see a genetic counselor isn’t for another month, or longer? Do you wait that long?
Depending on your extended family situation, you may be able to wait. But if not (if you’re not sure, ask us ), another option is sending a letter (we’ve provided a template for you below) that summarizes the situation and refers them to someone other than yourself for questions. We’ve found this to be the most stress-free solution, especially if you’re not comfortable talking to relatives. Ideally you would refer them to your genetic counselor, but if you haven’t met with one yet, you can refer them to us, which we’ve included in the letter.
Dear Family
The letter is in Word format and may be altered it to suit your situation. We hope this helps you deal with the delicate nature of explaining this complex information to family members, some of whom you may not even know. Keep in mind:
- It is not your responsibility to provide genetic counseling or to ensure your family members pursue testing.
- The letter in its original form is anonymous and does not refer to who the family member is that’s been diagnosed.
- You can sign you name in the letter, or it can be sent anonymously.
- If you need your relatives to help you locate other family members, include that information in the letter along with copies of an appropriate fact sheet that they can share with others — see our Info Series fact sheets and our Fragile X 101 ebook .
Below is the contents of the letter, which is available as a Word document:
To Whom It May Concern:
A member of your family has been identified as either having a condition called Fragile X syndrome (FXS) or being a carrier of a genetic change that could cause a Fragile X disorder (FXD). This means that other family members may also be carriers of this gene change and/or be at risk to have children with FXS. This letter has been sent to you to summarize information regarding the genetics of FXDs and Fragile X syndrome.
Fragile X syndrome is the most common form of inherited intellectual disabilities. It can occur in both males and females, though females often have milder features than males. Affected individuals can have intellectual disabilities, learning and behavioral disorders and/or autism. Other characteristics include repetitive speech, hyperactivity, and poor eye contact. Physical characteristics include large ears, flexible joints and a long face.
Fragile X is caused by a genetic change (mutation) in a gene called the FMR1 gene, which is on the X chromosome.
The Fragile X gene exists in a number of forms. An individual may carry a normal size gene, a “premutation” size gene or a “full mutation” size gene. Both males and females can inherit this gene in either the premutation or full mutation form. Often individuals with a premutation are referred to as “premutation carriers.”
Individuals with FXS have a full mutation gene. Individuals with a premutation are usually not affected with FXS but are at risk to have children or grandchildren with a full mutation.
Females have two X chromosomes. Women who have inherited the Fragile X gene in either the full or premutation form are at risk to have a child with FXS.
Males have one X chromosome inherited from their mother and one Y chromosome inherited from their father. Males who have inherited a full mutation from their mother will have FXS. Males who inherit a premutation will pass it on to all of their daughters and to none of their sons. In other words, all the daughters of male carriers will be carriers themselves.
Individuals who are premutation carriers are usually not affected, but they are susceptible to two other conditions:
- Fragile X-associated primary ovarian insufficiency (abbreviated FXPOI, pronounced “fax-poy”)—Seen in some women with the premutation, it results in early menopause and/or reduced fertility.
- Fragile X-associated tremor/ataxia syndrome (abbreviated FXTAS, pronounced “fax-tas”)—A late onset (over age 50) neurological condition, sometimes initially diagnosed as Parkinson’s disease, that is more common in males than females.
Therefore, even if you are not in your childbearing years, the possibility of being a Fragile X gene carrier has implications for your health, your children’s or your grandchildren’s health.
A DNA test for FXDs, called the “FMR1 DNA test,” has been available since 1991. This test is extremely reliable in detecting the premutation or full mutation of Fragile X. Since a member of your family has been identified as carrying this gene change, you and your children (if you have any), may also carry this changed gene. It is therefore recommended that you and/or your children contact a genetic counselor to discuss your family history and the advisability of genetic testing. Your physician or other health care provider can order this testing on your behalf.
Your options should you wish to discuss the contents of this letter:
- You can locate a genetic counselor in your geographical area at www.nsgc.org.
- You can find additional information on the NFXF website by reviewing the section for “Newly Diagnosed” under the Living With Fragile X heading on the main menu at fragilex.org
We hope this information is of help to you. Please feel free to use any or all of the resources described above and should you have any further questions, you can contact the National Fragile X Foundation by phone at (800) 688-8765 or by email at treatment@fragilex.org.
Sincerely,
XXXXXXXX
JUMP TO
You and Your Child
Accessing Services
Visit a Fragile X Clinic
See a Genetic Counselor
Telling Others
How to Reach Us


Families do best when there is open and honest communication about Fragile X. Here’s our tips on how and when to start the conversation.
Fragile X Informational Downloads
Browse our available information flyers designed to be easily printable on home and office printers. We created these so you can distribute them as needed.
How to Reach Us

Hilary Rosselot

Anna De Sonia

Robby Miller

Amie Milunovich

Kristin Bogart

Missy Zolecki

Kim Toman
Our staff (shown here), board of directors, committee members, and other important partners are here to serve you and all those living and working with Fragile X. Learn more about the people behind the scenes at the NFXF.
Availability
We’re here Monday thru Friday, 9AM to 5PM ET, with the usual holidays as exceptions. If you leave a phone message and would like us to return your call, please state your phone number clearly — and it’s a good idea to repeat it just in case.
Email: treatment@fragilex.org
Phone: (800) 688-8765
What to Expect
Whether you leave us a message, email us, or use our form below, one of our team members will reply and help you with your questions and concerns.
Availability
We’re here Monday thru Friday, 9AM to 5PM ET, with the usual holidays as exceptions. If you leave a phone message and would like us to return your call, please state your phone number clearly — and it’s a good idea to repeat it just in case.
Email: treatment@fragilex.org
Phone: (800) 688-8765
What to Expect
Whether you leave us a message, email us, or use our form below, one of our team members will reply and help you with your questions and concerns.
Meet Our Team ↓

Hilary Rosselot
Executive Director

Kristin Bogart

Missy Zolecki

Anna De Sonia

Robby Miller

Amie Milunovich

Kim Toman

Jaleesa Holden

Mandie Rush
More Ways to Connect

How Can We Help?
If you have questions about anything — we’d love to hear from you. You can reach out to Missy Zolecki directly, or submit your question or comment through our contact form here.
Missy Zolecki,
Director, Community Engagement
treatment@fragilex.org
Direct: (202) 594-8376
Toll-Free: (800) 688-8765

How Can We Help?
If you have questions about anything — we’d love to hear from you. You can reach out to Missy Zolecki directly, or submit your question or comment through our contact form here.
Missy Zolecki,
Director, Community Engagement
treatment@fragilex.org
Direct: (202) 594-8376
Toll-Free: (800) 688-8765
Last Updated: 10/01/2021