Fragile X–Associated Tremor/Ataxia Syndrome | FXTAS
Fragile X–associated tremor/ataxia syndrome was first described in five grandfathers of children with Fragile X syndrome in 2001 by Dr. Randi Hagerman and her colleagues at the MIND Institute, University of California, Davis. These men were generally healthy until the onset of the FXTAS-related symptoms.
For a few years prior to the first report, Dr. Hagerman and other Fragile X experts had been noticing a pattern of grandfathers of children with Fragile X syndrome diagnosed with:
- Parkinson’s disease
- Alzheimer’s disease
- Various “ataxias” (balance problems)
- Tremors (shakiness of the hands)
- Other neurological conditions
 Sometimes these men accompanied their grandchildren to the clinic where their symptoms were noticed, or it was reported when the family was giving family health histories.
Sometimes these men accompanied their grandchildren to the clinic where their symptoms were noticed, or it was reported when the family was giving family health histories.
Eventually, magnetic resonance imaging (MRI) exams were obtained on these men, and similar findings were noted among them. This information linked together:
- Their symptoms.
- Their genetic markers (the FMR1 premutation).
- The MRI changes in their brains.
Based on this data and a great deal of scientific consultation, Dr. Hagerman and her team introduced the term “FXTAS,” or Fragile X–associated tremor/ataxia syndrome, in 2003. Though it initially included only male carriers over the age of 50, females were later also found to have features of FXTAS, though the symptoms are usually milder and the condition is not seen as often.
Within a short time, individuals with no family history of Fragile X were being diagnosed with FXTAS at various medical clinics. These were FMR1 premutation carriers who did not have known family members with Fragile X syndrome and may not have known they carried the FMR1 premutation.
What is FXTAS
Fragile X–associated tremor/ataxia syndrome or FXTAS is an adult-onset neurodegenerative disorder, more common in males than females over 50 years of age with the Fragile X premutation. FXTAS is associated with tremors, balance problems, and other neurological signs. FXTAS progresses at varying rates in different individuals.
All individuals with FXTAS are premutation carriers of the FMR1 (Fragile X) gene (CGG repeats 55-200). The job of the FMR1 gene is to make protein (FMRP) that is important in brain development. Researchers believe that (for unknown reasons) having the premutation leads to the overproduction of FMR1 mRNA (which contains the expanded repeats). They believe that the high levels of mRNA are what cause the signs and symptoms of FXTAS, but more research is needed. Note: Not all premutation carriers will develop FXTAS, but all individuals with FXTAS have an FMR1 premutation. Researchers are investigating what other factors might contribute to FXTAS in FMR1 premutation carriers.
In its “full mutation” form the FMR1 gene causes Fragile X syndrome, a different, but genetically related disorder that is present from birth but is often undiagnosed or misdiagnosed for many years.
Female premutation carriers can also be affected by Fragile X-associated primary ovarian insufficiency (or FXPOI), another of the conditions associated with the change in the FMR1 gene.
Be a part of the solution.
Learn more about the INTERNATIONAL FRAGILE X PREMUTATION REGISTRY and join individuals with the premutation and their families to help advance — and encourage — deeper understanding and research into the premutation condition.
Be a part of the solution.
Learn more about the International Fragile X Premutation Registry and join individuals with the premutation and their families to help advance — and encourage — deeper understanding and research into the premutation condition.
Prevalence
 Among premutation carriers, about 40% of males older than 50 years and 8%-16% of women older than 40 years develop FXTAS.
Among premutation carriers, about 40% of males older than 50 years and 8%-16% of women older than 40 years develop FXTAS.
However, the risk of FXTAS in any given individual is influenced by their:
- CGG repeat size — A larger number of repeats increases the risk
- Sex — Men are at greater risk
- Age — Symptoms are more common at older ages
In women, the activation ratio, or percentage of cells expressing the premutation allele, may also play a role.
Considering all of these factors and literature to date, it is estimated that the lifetime prevalence of FXTAS in the general population is approximately 1 in 8,000. This indicates that FXTAS is significantly less common than essential tremor or Parkinson’s disease in older adults.
For men who are premutation carriers, the chance of developing core symptoms of FXTAS (tremor, problems with walking or balance) increases with age:
% Chance of Male Premutation Carriers
Developing Core Symptoms of FXTAS
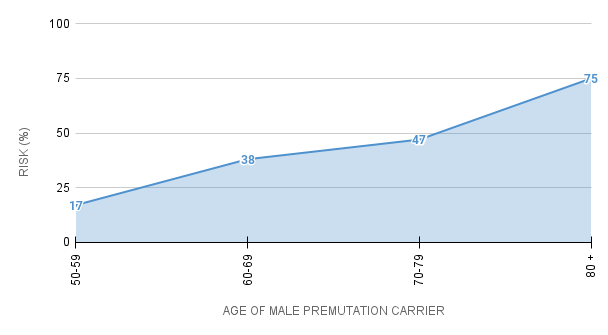
For men who are premutation carriers, the chance of developing core symptoms of FXTAS (tremor, problems with walking/balance) increases with age:
- Ages 50-59 the chance is about 17%.
- Ages 60-69 about 38%.
- Ages 70-79 about 47%.
- Over 80 years old, about 75% will develop symptoms of FXTAS.
Studies of females have found that about 8-16% of premutation carriers, within families already known to have someone with a Fragile X condition, develop some FXTAS symptoms. The symptoms in females tend to be milder.
FXTAS may be one of the most common adult onset, single-gene neurological diseases similar in prevalence to other neurodegenerative diseases such as ALS (Lou Gehrig’s disease); however, more studies within the general population will be necessary before the true incidence is known.
Learn more about prevalence of the three Fragile X disorders »
Signs & Symptoms
The symptoms of FXTAS are divided into minor and major clinical and MRI findings. The diagnosis is then categorized into definite, probable, or possible FXTAS. The criteria were developed primarily as a reflection of the presenting symptoms in men. As we learn more about FXTAS in females, the diagnostic criteria may become different for females, since they usually have milder symptoms. Both the type and severity of FXTAS symptoms vary among individuals. Some will have multiple symptoms that progress rapidly, others few symptoms that remain mild over many years.
There are also comorbid symptoms of FXTAS, which means they often occur in individuals with FXTAS but aren’t used to confirm the diagnosis (just as a sore throat is a symptom of strep throat, but cultures, fever, etc., are also used to make the diagnosis).
Major FXTAS Symptoms
- Intention tremor: A tremor of the hand when using utensils, writing instruments, reaching for or pouring something. The tremor is not as apparent at rest.
- Gait ataxias: Balance problems which may include falling, needed support when walking or going up/down stairs, trouble stepping on/off curbs, generalized instability, or display of a wide-based gait.
- MRI findings strongly associated with (but not unique to) FXTAS. These findings include white matter lesions involving middle cerebellar peduncles (MCP) signs.
- Neuropathology findings called “FXTAS inclusions” within brain cells.
Minor FXTAS Symptoms
- Parkinsonism (resting tremors).
- Short-term memory problems. This can be difficult to determine since it is natural for short-term memory to deteriorate as we age. However, in FXTAS it can change more rapidly than normal or may be more dramatic, such as forgetting what one ate, said, or did shortly after the event.
- Problems with “executive function” and decision-making. Executive function includes the ability to initiate and complete an activity, to adapt and change behavior as needed, and to anticipate and plan for new tasks and situations. Executive function allows us to anticipate outcomes, solve problems, and generalize from one situation to the next.
- MRI findings that are more general than those listed above, referred to as “lesions of cerebral white matter.” And other MRI findings indicating “moderate to severe generalized brain atrophy.”
Other FXTAS Symptoms
These are not considered to be official diagnostic criteria.
- Neuropathy or numbness/tingling of the extremities.
- Mood instability, irritability, explosive outbursts, personality changes.
- Cognitive decline, including loss of skills such as math, reading, etc.
- Autonomic functioning problems such as impotence and loss of bladder or bowel functions.
- High blood pressure, thyroid disorders, fibromyalgia (more common in females and very common in the general population).
Definite vs. Probable vs. Possible FXTAS
Definite FXTAS
- Individuals with one major clinical symptom (#1 or #2 under major symptoms above) and one major radiological symptom (#3 or #4).
- Any individual with the presence of FXTAS inclusions based on neuropathology.
Probable FXTAS
- Individuals with two major clinical symptoms (both #1 and #2 under major symptoms above).
- Individuals with one minor clinical symptom (#1, #2 or #3 under minor symptoms above) and one major radiological symptom (#3 or #4 under major symptoms).
Possible FXTAS
- Individuals with one major clinical symptom (#1 or #2 under major symptoms above) and one minor radiological symptom (#4 or #5 under minor symptoms).
- Any individual who may be a Fragile X carrier (with or without a family history of Fragile X) or who has symptoms in any of these three categories should be seen by a neurologist, movement disorders specialist, or psychiatrist familiar with FXTAS or the other Fragile X conditions.
Most Common Symptoms in Males
- Intention tremor: A tremor of the hand when using utensils, writing instruments, reaching for, or pouring something. The tremor is not as apparent at rest.
- Gait ataxias: Balance problems which may include falling, needed support when walking or going up/down stairs, trouble stepping on/off curbs, generalized instability, or display of a wide-based gait.
- Parkinsonism (resting tremors).
- Cognitive decline, including loss of skills such as math, reading, etc.
- Neuropathy or numbness/tingling of the extremities.
- Low blood pressure (orthostatic hypotension).
- Mood instability, irritability, explosive outbursts, personality changes.
- Problems with “executive function” and decision-making. Executive function includes the ability to initiate and complete an activity, to adapt and change behavior as needed, and to anticipate and plan for new tasks and situations. Executive function allows us to anticipate outcomes, solve problems, and generalize from one situation to the next.
- Difficulty learning new tasks.
- Autonomic functioning problems such as impotence and loss of bladder or bowel functions.
- MRI findings are strongly associated with (but not unique to) FXTAS. These findings include white matter lesions involving middle cerebellar peduncles (MCP) signs.
You may also be interested in our webinar “Fragile X-Associated Tremor/Ataxia Syndrome 101,” presented by neurologists Drs. Deborah Hall and Maureen Leehey who have been treating FXTAS patients over the last two decades. They provide an overview of the clinical features of FXTAS and treatment options, including surgery. Patients, caregivers, junior researchers, and others may benefit from the material in this presentation.
In Females
Females can experience the same neurological symptoms as males, but almost always with less severity. Most affected women have some degree of tremor and/or ataxia. While the psychiatric and mood disorders are also less frequent in females, they are at higher risk for anxiety and depression in general. Additional symptoms affecting some females include:
- Fibromyalgia and/or generalized muscle pain.
- Thyroid disorders, usually hypothyroidism.
- Seizure disorders.
Testing
 FXTAS only occurs in individuals who have a Fragile X (FMR1) premutation. Therefore, it is essential that anyone being considered for this diagnosis is tested for and confirmed as a premutation carrier. This involves DNA testing of the individual’s FMR1 (Fragile X) gene.
FXTAS only occurs in individuals who have a Fragile X (FMR1) premutation. Therefore, it is essential that anyone being considered for this diagnosis is tested for and confirmed as a premutation carrier. This involves DNA testing of the individual’s FMR1 (Fragile X) gene.
Treatment & Intervention
Each person with FXTAS is unique; each will have their own set of problems. While most will have hand shaking and balance problems, these will vary in severity and the need for treatment. Further, each affected person has a unique medical history, biological make-up, and personality.
While many of the FXTAS symptoms are neurological, many other body systems are also affected. To receive optimal care, it is best to have a medical care team that is knowledgeable about FXTAS. The team should include a neurologist and primary care physician at a minimum. Other specialists, e.g., in the areas of psychiatry, psychology, rehabilitation, urology, cardiology, and movement disorders neurology may also be needed.
There are three purposes of therapy for FXTAS:
- To reduce symptoms.
- To slow the progression of disease.
- To cure disease.
While there are no known treatments to slow progression or cure FXTAS, intense research is being done in this regard. There are a number of treatments that many affected persons have found helpful in reducing symptoms and disability.
In general, therapy that is most likely to help in any disease has been tested in well designed and executed clinical trials. However, FXTAS was only first published in 2001, so there has not yet been any treatments studied well enough to know if they definitely help.
Until we have proven therapies for FXTAS, it is reasonable to consider treatments that have been shown to reduce the same symptoms when they occur in other diseases. For example, many persons with FXTAS and shaking in their hands (ataxia tremor) will find that taking a medication that reduces hand shaking in another disease, e.g., essential tremor, is helpful.
The symptoms of FXTAS are known to vary from one person to another; so, the best treatment options vary from person to person. Useful treatments for FXTAS include:
- Medications
- Psychological and genetic counseling
- Rehabilitative treatments such as speech, occupational and physical therapy
- Gait training
- Surgery
- Family supportive services and counseling are also important
FXTAS Clinics
FXTAS Clinics are members of the NFXF’s International FXTAS Consortium (IFC) and specialize in FXTAS. They are comprised of doctors (primarily neurologists and movement disorder specialists), therapists, researchers, and other specialists who treat FXTAS by utilizing the best available scientific knowledge about the known causes of FXTAS. While there is currently no cure for FXTAS, specialists may be able to lessen the severity or slow the progression of symptoms.
FXTAS vs. FXS
FXTAS and FXS are not the same condition. Both are caused by mutations of the same gene, the FMR1 gene, but they are caused by different changes in this gene. FXS is caused by a full mutation of the FMR1 gene, FXTAS by a premutation of the FMR1 gene.
Even more important in distinguishing between FXS and FXTAS are the different features, age of onset, and diagnostic criteria of the two conditions.
Fragile X Syndrome (FXS)
FXS is present (though often not diagnosed) at birth. Children display features of the condition early in life, usually noticed by family members in infancy, toddlerhood, or early childhood. These features include:
- Delays in cognitive, language, and social development.
- Behavioral issues.
- Physical characteristics such as large ears, large testes in males, flexible joints and a long face (more common as children get older).
Fragile X-associated Tremor Ataxia Syndrome (FXTAS)
FXTAS develops in adulthood—usually after age 50. The symptoms may appear slowly and develop over years or decades. Individuals with FXTAS usually are healthy, usually with normal cognitive skills prior to the onset of the condition. They have no unique physical characteristics and did not experience the developmental delays in childhood that are seen in FXS.
Other Differences
- In FXS, the FMR1 gene is fully methylated.
- In FXTAS, the FMR1 gene is in its normally unmethylated state.
- FXS is diagnosed by molecular (DNA) testing of the FMR1 gene. Virtually all boys with a full mutation have FXS and about 50% of girls with a full mutation have features of FXS.
- FXTAS is diagnosed by fulfilling certain criteria. These include being an FMR1 premutation carrier, the appearance of neurological features such as ataxia (balance problems), tremors, and other symptoms, and MRI findings.
Additional Help & Resources
With FXTAS being a relatively new disorder, there may not appear to be as many services and professionals available as there is for other medical conditions. However, a number of support services and informational materials may be of value to those impacted by FXTAS, some of which address symptoms common to other medical conditions such as Parkinson’s. We are on the lookout for more services and will continue to update this list below. In the meantime, we welcome reader’s recommendations.
- FXTAS Clinics »
- Movement Disorder Society »
- International Guide to Movement Disorder Patient Advocacy Groups and Foundations »
- Caregiving recommendations for those with FXTAS from the Colorado Fragile X Consortium »
- Treatment of Fragile X-associated tremor ataxia syndrome (FXTAS) and related neurological problems »
- Consensus of the FXTAS Task Force and the Fragile X Clinical & Research Consortium »
- Fragile X-Associated Tremor/Ataxia Syndrome: Clinical Features, Genetics, and Testing Guidelines »
- Facebook Support Group for people living with FXTAS and their caregivers.
- International Parkinsons and Movement Disorder Society »
- International Guide to Movement Disorder Patient Advocacy Groups and Foundations »
- Caregiving Recommendations for those with FXTAS from the Colorado Fragile X Consortium »
From the fragile x info series
Fragile X Info Series flyers are designed to be easily printable on home and office printers. We created them so you can distribute them as needed, whether it’s for a neighbor, students at school, your own reference, or you work at a clinic and want to share information with new families. Whatever the cause, they are meant to be informative and shareable.