Consensus of the Fragile X Clinical & Research Consortium
Sleep in Children With Fragile X Syndrome
Reading Time: 17 min.—|—Last Updated: Oct. 2012—|—First Published: June 2011—|—Download PDF
In general, children with neurodevelopmental disabilities have higher rates of sleep disturbances than the general population, reaching as high as 80% prevalence. Parents of children with Fragile X syndrome of all ages report one-third to one-half of their children have sleep problems. Gender, socioeconomic status, and family composition do not play a role in prevalence rates. Children with Fragile X syndrome who are reported to have higher rates of sleep disturbances typically include younger children, although sleep problems are reported at higher rates across all age groups and in those children with multiple co-occurring conditions (i.e., ADHD, developmental delays, autism, anxiety).
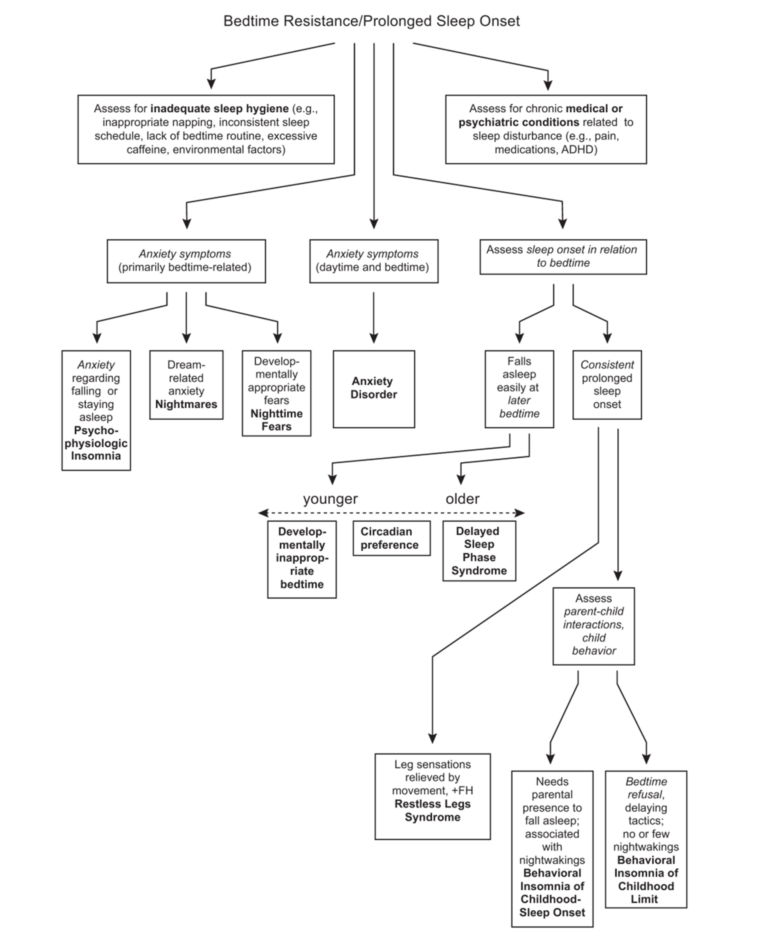
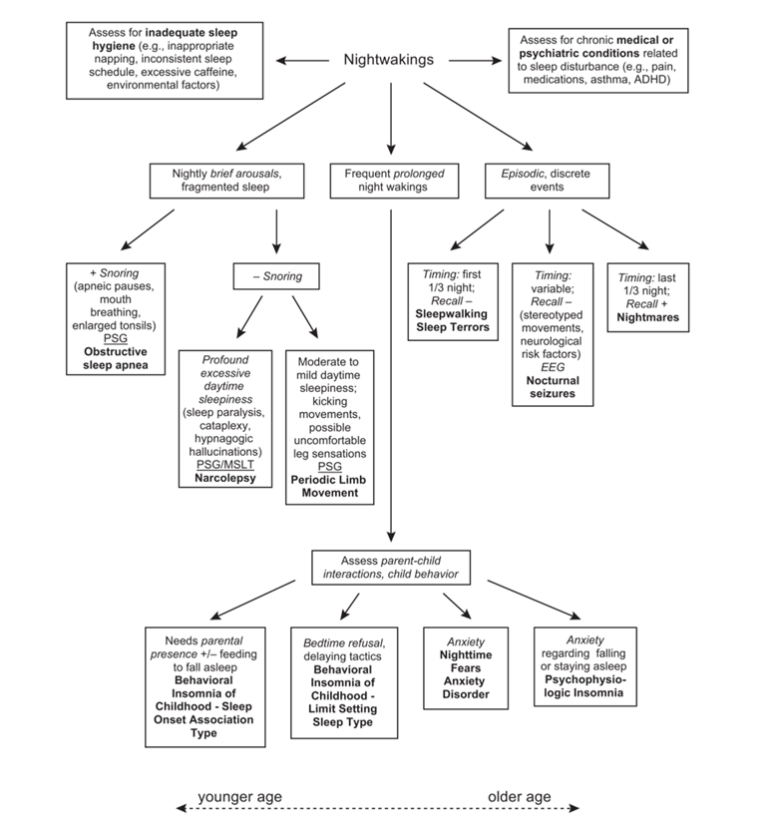
Sleep disturbances can be categorized into three main presentations:
- Insomnias, which include problems falling asleep or maintaining sleep
- Parasomnias, which are abnormal sleep-related behaviors such as sleepwalking, sleep terrors, and enuresis
- Sleep-related breathing disorders, including obstructive sleep apnea.
Depending on the presentation and primary disorder, treatment may include behavioral, pharmaceutical, and surgical interventions.
Diagnosis
Typically a child’s sleep pattern is recognized as problematic when it becomes a disturbance to family functioning. However, many parents of children with special needs may feel they should “just live with” the problem since it is assumed to be part of the disorder. Hence they may never volunteer their concerns at a clinical visit.
The clinical visit should include a careful history of sleep habits with leading questions such as:
- Do you have any concerns regarding your child’s sleep?
- Does your child take more than 30 minutes to fall asleep at bedtime?
- Once asleep, do they stay asleep?
- Are they afraid to sleep alone?
- Does your child seem excessively sleepy during the day?
- Have you heard your child snore or stop breathing during the night?”
Many clinics employ standardized parent questionnaires such as the Child’s Sleep Habits Questionnaire (CSHQ)↗. It is a brief assessment that helps identify sleep habits and target problematic areas. A two-week sleep diary often reveals patterns that can help lead to effective treatments. In addition, attention to physical and systemic findings, such as cardio-respiratory disease, facial or pharyngeal abnormalities, and obesity, can be a focus of the physical examination. Once data collection is complete, the clinician will need to decide if the child needs a more detailed evaluation (i.e., ENT, EEG, sleep clinic), or whether treatment can be implemented within the scope of the office practice.
Current Treatment Recommendations
Treatment for insomnias and most parasomnias can begin within the clinical practice. Health promotion strategies that include education regarding healthy sleep habits within a “developmental framework” can improve sleep hygiene. Some parents benefit from a further understanding of sleep physiology and psychology, such as knowing about sleep stages and the environmental cues called “zeitgebers.” Monitoring daytime behaviors — including meals and other activities — can help regulate nighttime schedules. Appropriate treatment of co-existing conditions (i.e., ADHD, anxiety) will have positive secondary effects on sleep promotion.
Very few studies have investigated the effectiveness of sleep medication in children with Fragile X syndrome. However, multiple studies on the effectiveness of melatonin and Clonidine have been completed on other children, with and without neurodevelopmental disabilities.
The literature promotes the efficacy of melatonin for reducing sleep onset latency. Typically, melatonin is given one hour prior to expected bedtime. Typical dosing begins with the lowest dose (0.5 to 1 mg) with incremental increases up to 3 mg. The use of melatonin in children with special needs has been reported to range from 0.5 mg to 10 mg. Only one study showed an increase in seizure activity in a child with a significant neurologic condition and seizures. Melatonin also comes in an extended-release formulation and can help with sleep maintenance. Suggesting the purchase of pharmaceutical-grade melatonin is recommended since melatonin is not regulated by the FDA and may vary in strength and purity.
Although off-label, the alpha-agonist Clonidine is a widely used medication in pediatrics for insomnia. It is typically prescribed beginning at 0.025 mg to maximum dosing of 0.4mg/day. It has also been used to treat ADHD symptoms, especially in younger children. Frequently reported side effects include drowsiness, headache, insomnia, and hypotension. Several drug-to-drug interactions have been documented. It should not be used with a history of cardiovascular disease or depression. Rebound hypertension can occur upon abrupt discontinuation.
Summary
Sleep problems can be more frequent in children with developmental disabilities, including Fragile X syndrome. The clinician needs to provide a thorough interview or validated assessments as well as a focused physical examination in order to identify specific patterns and decide appropriate next steps.
Sleep is a complex interaction of health condition, environment, and emotions; all these factors must be taken into account in order to help families achieve the good night’s sleep that they so deserve. Children, especially those with an already compromised nervous system, need their sleep for optimal development and functioning. Ongoing support toward that end from medical providers can help play an important role
Authors’ Note
This guideline was authored by Rebecca Kronk, PhD, CRNP, and was reviewed and edited by consortium members both within and external to its Clinical Practices Committee. It has been approved by and represents the current consensus of the members of the Fragile X Clinical & Research Consortium. Learn more about the NFXF team.
The Fragile X Clinical & Research Consortium was founded in 2006 and exists to improve the delivery of clinical services to families impacted by any Fragile X-associated disorder, and to develop a research infrastructure for advancing the development and implementation of new and improved treatments.
Funding: This project was made possible by Cooperative Agreement U01DD000231 from the Centers for Disease Control and Prevention to the Association of University Centers on Disabilities (AUCD) and RTOI 2008-999-03 from AUCD to W.T. Brown in support of the National Fragile X Clinical and Research Consortium. The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Questions?
If you’re a parent or caregiver and have questions about the information presented here, we’d love to hear from you! You can reach out to Missy Zolecki using the contact info or our contact form below.

Missy Zolecki,
Community Empowerment
treatment@fragilex.org
(800) 688-8765