What is FXPOI?
Fragile X-associated primary ovarian insufficiency, one of three known Fragile X-associated conditions caused by changes in the FMR1 gene, is a condition in which the ovaries are not functioning at full capacity in an individual with the FMR1 premutation. It can cause infertility, early menopause, and other ovarian issues. FXPOI occurs in about 20% of women with the FMR1 premutation.
Fragile X-associated primary ovarian insufficiency is also known as FXPOI and is pronounced faks-poi.
Ovaries form part of a female’s reproductive system. They contain all of a female’s eggs. The eggs are released to the uterus each month midway through a female’s menstrual cycle, where they wait to be fertilized. If not fertilized, they leave the body in the menstrual period.
Ovaries also produce and release hormones that are important in fertility and for the preparation and maintenance of the eggs. As females age, their ovaries slowdown in overall function, including their ability to maintain and release eggs. The eggs themselves age and may not be healthy enough for fertilization and development of a baby.
The ovaries in females with FXPOI do not function to full capacity and may resemble ovaries of an older woman, both in the number and quality of available eggs.
FXPOI Resource

FXPOI Prevalence
About 20%–30% of women with the Fragile X premutation develop FXPOI over their reproductive life span, compared with only 1% in the general population.[1]
On average, women with the Fragile X premutation experience natural menopause at an earlier age compared to those without the Fragile X premutation. On average, females with the Fragile X premutation may experience menopause about 5 years earlier than those in the general population, who experience menopause between 45 and 55 years old.[2, 3]
Approximately 3% of women who carry the premutation will have menstrual cycle irregularities in their teens or twenties due to FXPOI, and 1% of women who carry the premutation will stop having periods before the age of 18.[4]
About one-third of women with FXPOI, equivalent to 7% of women who carry the premutation, stop having periods at or before age 29.[5]
Not all women with a premutation experience FXPOI. One well-documented risk factor is the premutation repeat size: the highest risk for ovarian dysfunction is for females carrying premutation alleles in the 70-100 CGG repeat range. Women with repeats less than five or greater than 120 did not have increased risk for FXPOI compared to women without the Fragile X premutation.
FXPOI Signs & Symptoms
Common symptoms of FXPOI include absent or irregular cycles, “sub-fertility” or infertility, hot flashes, and premature ovarian failure (POF), which is the complete cessation of menstrual periods before the age of 40. In the wider range of FXPOI symptoms, premature ovarian failure is at the more severe end of the spectrum.
Women with the FMR1 premutation can have typical ovarian function, but can still go through early menopause, which is menopause occurring between 40 and 45 years of age (menopause typically occurs between 45 and 55 years old).
Even though women with FXPOI may develop symptoms similar to those of menopause, FXPOI differs from menopause in some important ways:
| Women with FXPOI | Women who have completed menopause |
| Can still get pregnant in some cases because their ovaries may occasionally function to release viable eggs. | Cannot get pregnant because their ovaries no longer release eggs. |
| Can experience a return of menstrual periods. | Cannot have menstrual periods again. |
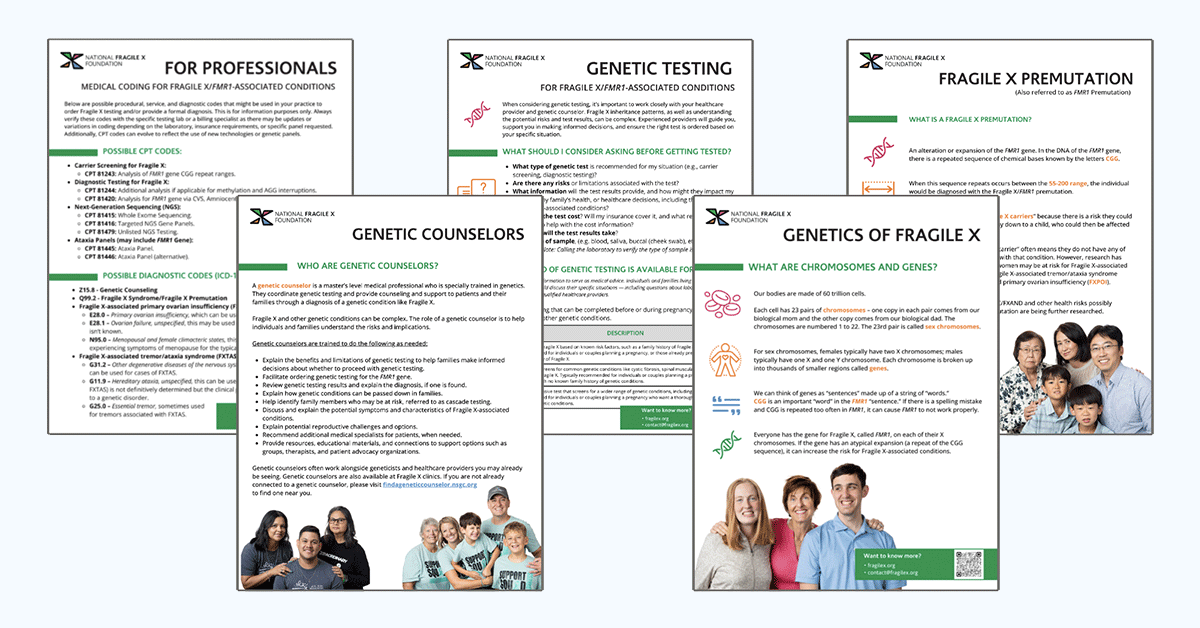
Testing for FXPOI
All women who have FXPOI have an FMR1 premutation. All females with the FMR1 premutation should keep a log of their menstrual cycles and note any unusual patterns, missed cycles, abnormally long cycles (more than 35 days), or short cycles (less than 21 days). Also note any other physical changes such as hot flashes, insomnia, vaginal dryness and/or decreased libido, or increased anxiety.
If you are experiencing FXPOI symptoms and haven’t been tested, you should arrange with your physician to have FMR1 genetic testing. Any physician or genetic counselor can order testing for Fragile X.
If you can’t find a genetic counselor in your area, call us at (800) 688-8765 or visit the National Society of Genetic Counselors.
If you have already been tested and are a confirmed carrier of the FMR1 premutation, you should alert your physician to the risk of FXPOI. Some physicians might not be aware of this condition. You can explain that the American Society for Reproductive Medicine and American College of Obstetrics and Gynecology recommends that all women with ovarian insufficiency or elevated FSH levels have FMR1 testing.
If you are concerned that you might have FXPOI, talk to your physician about having your FSH, a hormone that reflects ovarian function, measured. FSH levels increase as you approach menopause or if your ovaries are not functioning properly for your age.
FXPOI Treatment & Intervention
Many women with the FMR1 premutation can get pregnant. And, all women with the FMR1 premutation are at risk to have children with FXS. Women with the Fragile X premutationare encouraged to meet with a genetic counselor to understand and discuss reproductive issues and options.
Some women with the FMR1 premutation are initially identified because they have fertility problems and are considering fertility treatment.
If you conceive naturally, you have the option of prenatal testing through amniocentesis or chorionic villus sampling (CVS) to evaluate the genetic status of your pregnancy.
If you are experiencing fertility challenges, you can discuss various assisted reproductive options with your OBGYN/reproductive endocrinologist, including IVF with your own eggs, IVF with eggs donated by a non-carrier, attempting to get pregnant naturally, and/or adoption.
Fragile X-Associated Primary Ovarian Insufficiency (FXPOI)
All women diagnosed with primary ovarian insufficiency should undergo testing for the Fragile X premutation, even if they have no family history. Since not all women with the premutation will develop FXPOI, itʼs crucial to identify risk factors that can help predict its onset.
Genetic Counseling and Family Support
Genetic counseling includes family and medical histories to assess the chance of carriers (premutations) throughout a family’s lineage.
More FXPOI Resources