Early Childhood Developmental and Educational Guidelines for Children with Fragile X Syndrome
Consensus of the Fragile X Clinical & Research Consortium
For all children within the early childhood age range (birth to 5 years) and especially for young children with identified disabilities associated with a diagnosis, like Fragile X syndrome (FXS), inclusive, nurturing, and developmentally appropriate environments and caregiving are essential to growth and development. The national Division for Early Childhood (DEC) of the Council for Exceptional Children identified eight recommended practices in early intervention and early childhood special education that are salient to young children with FXS and their families (DEC, 2014).
While these recommended practices are equally important, this document will focus on Assessment, Family, Environment, and Transition.
1. Leadership
2. Assessment
3. Environment
4. Family
5. Instruction
6. Interaction
7. Teaming & Collaboration
8. Transition
Early Intervention
The Early Intervention (EI) program for families with infants and toddlers (birth to 3 years) with disabilities is Part C of the Individuals with Disabilities Education Act (IDEA) of 2004. The services in this federal law may include occupational therapy, speech/language therapy, and developmental, play, and/or behavioral interventions. Other services related to feeding, vision, or hearing may also be available. Services may occur within the child’s natural environments, which include the family home, child care program, or community settings (i.e., library, play group, playground). Services may be delivered by a transdisciplinary team, meaning that one primary provider will deliver all the services and then consult/collaborate with other team members with different areas of expertise as needed. The team members release their role to the primary provider so that the family is not inundated with many different providers at different times. The family and other care providers are an integral part of the team as the primary provider works closely with those individuals that spend the most time with the young child. The primary provider works with the family and other care providers to implement the strategies within the child’s daily routines. The primary document for families enrolled in their state’s EI program is call the Individualized Family Service Plan (IFSP). This document identifies the child and family’s strengths, needs, and functional outcomes and is reviewed every six months (DEC, 2010).
Early Childhood Special Education
Early childhood special education (ECSE) services are for preschool-aged children (3–5 years) with disabilities and implemented by public school systems. This program is Part B (Section 619) of the Individuals with Disabilities Education Act of 2004. These services typically occur in preschool or child care environments with licensed teachers and an interdisciplinary team (e.g., early childhood special education teacher, speech-language pathologist, occupational therapist, school psychologist). The Individualized Education Program (IEP) is the legal document that guides the child’s educational program and services. The IEP is developed by an interdisciplinary team including teachers, parents, and other professionals based on the child’s needs. Constructed on the regulations set forth in the Individuals with Disabilities Education Act (IDEA), the plan must be revised annually (parent or school personnel may request an IEP review meeting at any time). Critical components of the IEP include parent involvement, goals, and objectives related to the child’s current development and next steps, and intentional accommodations and modifications. Accommodations are strategies used by the teacher to “level the playing field” for children with disabilities and provide equitable access to the curriculum, meaningful participation, and adequate support. Examples of accommodations may include providing a visual schedule, extra adult or peer support, or breaks for movement (DEC, 2010). Modifications are changes to the curriculum or expectations for the child, which may include simplification of tasks or altered schedules that are important for the success of children with FXS. [See IEP checklist at the end of this document].
Assessment through Child Find Activities
The heart of the individualized program is a determination of need based on formal (standardized and norm-referenced) and informal (observations, play-based, authentic) assessments. The assessment and individualized plan or program provide the basis for goals, objectives, accommodations, modifications, and subsequent services that are necessary to meet the child and family’s needs and next steps (McLean, Hemmeter & Snyder, 2014; National Research Council, 2008).
Child find activities are an IDEA requirement to locate and identify children (birth to 21) with disabilities. The screening and assessment processes associated with child find activities are at no cost to families and intended to be responsive to families’ needs and schedules. Some school districts have child find teams that are responsible for identifying and evaluating children birth to 5 years. They have the responsibility to use appropriate assessment methods to identify children and families’ strengths and needs. Child find teams are often transdisciplinary teams that use authentic play-based assessment methods to evaluate the child’s holistic development. Authentic assessment methods include a process to collect information about the child’s development through a variety of methods, including family interviews, direct observation, and facilitated play with the child with familiar toys, materials, caregivers, and during daily routines. Standardized and norm-referenced assessments are also used with young children to determine if they are eligible for early intervention or early childhood special education services.
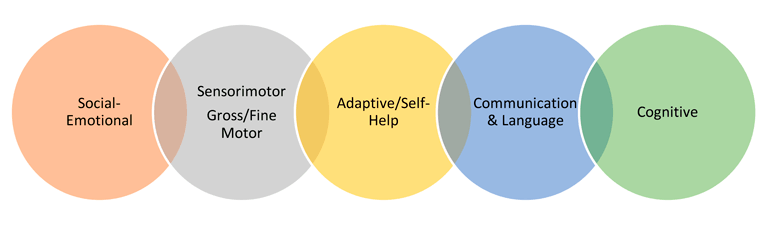
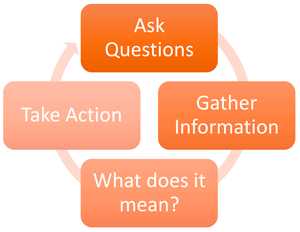 Early Childhood Assessment: Assessments for young children with FXS should be an authentic process that happens over time, with familiar caregivers, in familiar environments (see previous two paragraphs). There are diverse types of assessments that can be used to measure the developmental progress of children in the following developmental domains: cognition, physical & sensory motor, communication/language, and social/emotional. Information may be obtained from a variety of sources, such as parents, teachers, and other professionals (e.g., speech therapists, occupational therapists, physical therapists) to understand the whole child. The assessment may include a developmental history, observational checklists, and specific formal assessment instruments. Some assessments are play based, others may be more formal. The purpose of assessment is to promote children’s learning and development, identify special services, and monitor progress (McLean, Hemmeter & Snyder, 2014).
Early Childhood Assessment: Assessments for young children with FXS should be an authentic process that happens over time, with familiar caregivers, in familiar environments (see previous two paragraphs). There are diverse types of assessments that can be used to measure the developmental progress of children in the following developmental domains: cognition, physical & sensory motor, communication/language, and social/emotional. Information may be obtained from a variety of sources, such as parents, teachers, and other professionals (e.g., speech therapists, occupational therapists, physical therapists) to understand the whole child. The assessment may include a developmental history, observational checklists, and specific formal assessment instruments. Some assessments are play based, others may be more formal. The purpose of assessment is to promote children’s learning and development, identify special services, and monitor progress (McLean, Hemmeter & Snyder, 2014).
Types of Assessments:
- Observation: Watching children to know more about their development, learning, and behavior.
- Assessment: Ongoing process of observing, recording, and documenting a child’s actions, skills, and behaviors.
- Evaluation: Comparison of information gathered against a standard set of criteria.
- Interview: Information about how the child performs, strengths and needs as perceived from the parent or a provider can help round out the overall assessment and are sometimes formal interviews as part of Evaluation, or are used to supplement the Observation and Assessment.
Eligibility of Services: To determine the child’s eligibility for services, a multidisciplinary or transdisciplinary evaluation must first be administered by a team that may include speech-language pathologists, audiologists, occupational therapists, physical therapists, psychologists, social workers, and early intervention specialists. The disability category that most children with FXS may qualify for is called Child with a Developmental Delay. This disability category is for young children up to 9 years with a delay in one or more developmental delays. A diagnosis of Fragile X syndrome may enable the child to receive services without an evaluation because FXS is a diagnosis that has been shown through research to be associated with developmental delays and disabilities. Although, the team may want to complete a play-based evaluation to determine the child’s strengths, needs/next steps, likes and dislikes so an individualized and meaningful plan can be developed. Each state may have different criteria for disability categories and families should be aware of their state’s criteria.
Family
Families are an integral part of a child’s development and the active participation of families in decisions related to their children’s assessment, intervention, and ongoing services are crucial. Each family’s culture, customs, and priorities should be met with trusting and respectful partnerships. Parents are considered a child’s first teacher, and therefore are an integral part of each step of the process. The DEC Recommended Practices (2014) identify three themes related to families that include:
- Family-centered practices: Practices that treat families with dignity and respect are individualized, flexible, and responsive to each family’s unique circumstances; provide family members complete and unbiased information to make informed decisions; and involve family members in acting on choices to strengthen child, parent, and family functioning.
- Family capacity-building practices: Practices that include the participatory opportunities and experiences afforded to families to strengthen existing parenting knowledge and skills and promote the development of new parenting abilities that enhance parenting self-efficacy beliefs and practices.
- Family and professional collaboration: Practices that build relationships between families and professionals who work together to achieve mutually agreed upon outcomes and goals that promote family competencies and support the development of the child.
These practices and themes should be intentional and ongoing.
Environment
Inclusive early childhood environments refer to any natural setting in which children without disabilities play, learn, interact with others, and develop relationships. These environments could be families’ homes, private child care programs, public or private preschools, or family child care homes. Community organizations are also identified as natural environments for all children, which include playgrounds, libraries, play groups, and community centers.
Recently, the U.S. Departments of Education and Health and Human Services released a policy statement about including young children with disabilities in early childhood environments. This policy supports the notion that children with and without disabilities benefit from interacting and playing together.
Inclusion in early childhood programs refers to including children with disabilities in early childhood programs, together with their peers without disabilities; holding high expectations and intentionally promoting participation in all learning and social activities, facilitated by individualized accommodations; and using evidence-based services and supports to foster their development (cognitive, language, communication, physical, behavioral, and social-emotional), friendships with peers, and sense of belonging. This applies to all young children with disabilities, from those with the mildest disabilities, to those with the most significant disabilities.
(U.S. Department of Health & Human Services and the U.S. Department of Education, 2015, p. 3).
Within all early childhood environments, it is important for teachers and families to think about strategies within the physical, social, and temporal environment so that young children with FXS have meaningful access, participation, and support in their environments. Quality inclusive environments start with a universal design for learning that means EC environments should be designed and planned for children with the most significant needs first and those accommodations will benefit all children. Research supports inclusion for children with and without disabilities.
Transition
The transition process indicates a change in services and environments for young children with disabilities and can be a very stressful time for families. There are many unknown factors because families have yet to experience this process. There are two transition processes that are relevant to early childhood. The first process is from early intervention (infant/toddler) services to early childhood special education (preschool) services. The primary change of this transition is the shift of focus from the family to the child and the delivery of services within natural environments (i.e., family home) to an educational setting. The second process is from preschool to kindergarten (school-age). The primary change of this transition is from play-based interventions to academic interventions. While these shifts are evident in many programs and communities, it is best practice to continue family-focused and play-based interventions throughout the preschool and early school-age years (DEC, 2010). The following are some strategies that may help the transition process for children and families.
- Visit the new school/program—play on the playground, walk through the halls (with and without other children), check out the classroom, bathrooms, cafeteria, etc.
- Collaborate with providers to set up a meeting between the sending and receiving programs.
- Collaboratively develop a transition plan in which the team (i.e., families, teachers, and providers) discusses the child’s current skills, next steps, expectations, health, and safety factors within the new environment.
Early Childhood Intervention & Services
The following is a compilation of intervention, services, and assessments that are often provided to early childhood (birth to 5 years) children with FXS. This list is simply a guideline and should not be viewed as exhaustive.
| Developmental & Educational Services Chart | —Recommendations— | |
| Intervention & Service Components (Each component is described in more detail following chart) |
Birth to 3 Years | 3–5 Years |
| Transdisciplinary Team | Recommended | Recommended |
| Developmental Intervention (i.e., play, cognitive, literacy and early education supports) |
Recommended | Recommended |
| Psychological Services (i.e., social, emotional & behavioral supports, or Behavioral Intervention Plan) |
Recommended | Recommended |
| Speech & Language Therapy (i.e., communication/language, augmentative & pragmatic supports) |
Recommended | Recommended |
| Physical Motor Services (i.e., occupational and physical therapy) |
Recommended | Recommended |
| Individualized Family Service Plan (IFSP) (see above) | Every 6 Months | N/A |
| Individualized Education Program (IEP) (see above) | N/A | Annually |
| Health Care Plan | As Needed | As Needed |
| Safety Plan | As Needed | As Needed |
| Transportation | As Needed | As Needed |
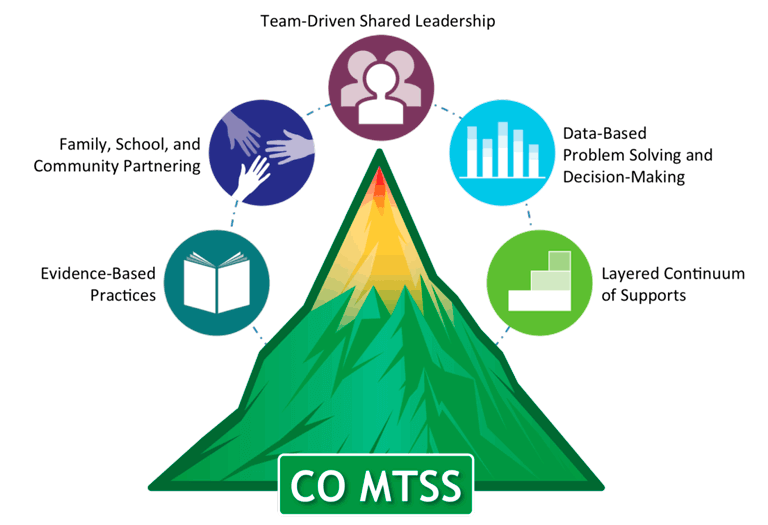
| Multi-Tiered System of Supports (MTSS) (includes Response to Intervention & Positive Behavior Intervention Supports) |
As Appropriate | AsNeeded |
| Sensory Integration Intervention within Occupational Therapy | As Needed | As Needed |
| Social Skills Training | As Needed | As Needed |
| Early Childhood Assessment (see above) | Recommended | Recommended |
| Functional Behavioral Assessment | As Needed | As Needed |
| Applied Behavior Analysis (ABA) Therapy | As Needed | As Needed |
| View additional educational information. | ||
Reviewed annually based on current levels of functional development.
Description of Intervention & Service Components
Transdisciplinary Team Approach: “Transdisciplinary service is defined as the sharing of roles across disciplinary boundaries so that communication, interaction, and cooperation are maximized among team members.” (King et. al, 2009, p. 211) This type of approach is preferable to a single provider approach because young children’s development changes so rapidly and all developmental areas are interrelated. Teams may include families, Early Childhood Special Education (ECSE) Teacher/Specialist, Speech/Language Pathologist, Occupational Therapist, Physical Therapist, School or Clinical Psychologist, and/or Social Worker. The make-up of the team depends upon the needs of the child. The “primary provider” is one of the professionals who addresses the primary needs of the child. That primary provider is the team lead and provides all the services to the child and family and then consults with the rest of the team on a regular basis. The other team members release their role and support the primary provider so that the child and family only interact with one provider at a time. This approach is beneficial to families because it can be overwhelming to manage multiple services and providers for their children. Using this approach simplifies the services and focuses on the primary needs of the child, while also supporting overall development (Pletcher & Younggren, 2013).
 Developmental Intervention (i.e., play, cognitive, literacy, early education supports): Developmental intervention is typically delivered by an early childhood special education teacher or specialist through a team-based approach in the home or classroom environment. This type of intervention focuses on play skills related to cognitive development to enhance attention, memory, problem-solving, early math, and literacy skills (Linder, 2008). Various kinds of play may include sensory play (i.e., water, sand, movement), manipulative play (i.e., blocks, Legos, small action figures), dramatic play (i.e., dress up, thematic), physical play (i.e., ball, running, hopping, climbing, bicycle) and storybook reading. Strategies focus on nurturing adult-child interactions within everyday routines, responsive caregiving, face-to-face positioning, and developmentally appropriate activities that capture the child’s attention. The provider works directly with the child and coaches or guides the primary adults that support the child every day within the natural environments, so that skills can be practiced multiple times a day so that generalization occurs across environments, people, and situations.
Developmental Intervention (i.e., play, cognitive, literacy, early education supports): Developmental intervention is typically delivered by an early childhood special education teacher or specialist through a team-based approach in the home or classroom environment. This type of intervention focuses on play skills related to cognitive development to enhance attention, memory, problem-solving, early math, and literacy skills (Linder, 2008). Various kinds of play may include sensory play (i.e., water, sand, movement), manipulative play (i.e., blocks, Legos, small action figures), dramatic play (i.e., dress up, thematic), physical play (i.e., ball, running, hopping, climbing, bicycle) and storybook reading. Strategies focus on nurturing adult-child interactions within everyday routines, responsive caregiving, face-to-face positioning, and developmentally appropriate activities that capture the child’s attention. The provider works directly with the child and coaches or guides the primary adults that support the child every day within the natural environments, so that skills can be practiced multiple times a day so that generalization occurs across environments, people, and situations.
Psychological Services (i.e., social, emotional, behavioral supports): Social, emotional, and behavioral supports at a young age require a play-based approach, as mentioned above. Services may be delivered by a school/clinical psychologist or an ECSE through a team-based approach. Providers and families may work on developing skills such as expressing emotions, flexibility in transitions, regulating emotions and behaviors, and interacting with others (Linder, 2008).
- At times, a Behavior Intervention Plan (BIP) is developed to address specific behaviors that may interfere with the child’s ability to learn. The plan should include specific techniques and strategies and be included in the child’s IEP. A vital component of the BIP is the progress monitoring and crisis intervention. There is an accountability factor built-in so that a BIP does not continue to be implemented if it is ineffective.
- Social skills training and support may be incorporated into the child’s daily routine through modeling and turn-taking with an adult or through structured peer group play activities. The use of visuals and social stories are effective strategies to help young children with FXS learn to manage their behavior (Dunlap, Wilson, Strain & Lee, 2013).
The graphic (above/right) is from the Center on the Social and Emotional Foundations of Early Learning and is a framework of evidence-based practices for supporting young children with challenging behaviors.
Speech & Language Therapy (i.e., communication/language, augmentative & pragmatic supports): Communication services are typically delivered by a Speech-Language Pathologist (SLP) through a team-based approach. Providers focus on the child’s ability to understand and use language effectively. The primary strategy for young children with FXS is to talk with them during daily routines by playing games, reading stories, pointing to objects and talking about them, using short phrases, and providing gestures and/or sign language. Families should encourage all forms of communication, such as vocalizations and gestures. Imitation, modeling, and expanding on the child’s language through every day activities (i.e., meals, toileting, dressing, going out, play, reading) are effective strategies to enhance communication and language (Lane & Brown, 2016).
Augmentative Communication is an alternative method of communication used for individuals with speech and language disabilities. It may include gestures, communication boards, pictures, symbols, drawings, or the use of an assistive technology device. Pragmatic language support is very important for children with FXS as they may benefit from explicit instruction in social language. For example, they may need assistance with using language for different purposes, adjusting language to meet the needs of the listener or situation, or for following the rules of conversation. Speech therapy may aid in the development of functional communication skills and improve a child’s pragmatic use of language. Improved communication skills may facilitate the building of peer relationships. Sometimes, children with FXS have oral motor delays that affect their ability to produce certain sounds and sequences of sounds. This can interfere with how they say certain sounds and words, referred to as articulation or speech intelligibility (Lane & Brown, 2016).
Physical Motor Services (i.e., occupational and physical therapy): Physical motor services may include gross (large muscle) and fine (small muscle) motor activities, as well as sensory activities.
- Occupational therapy (OT) may be recommended to address fine motor-difficulties-related manipulation of small toys or objects that build the strength needed for handwriting and dressing. This may serve to reduce anxiety and frustration related to academic tasks when in school. Activities such as playing with playdough, drawing/scribbling with crayons or makers, stringing beads or putting together Legos, provide young children with FXS opportunities to reach, grasp, release, and refine fine motor skills in functional ways. Occupational therapy may be utilized to address adaptive functioning or self-help skills such as dressing, grooming, or feeding. It may also be used to help determine the need for compensatory tools and strategies (e.g., use of the computer and keyboarding skills) to optimize functioning later in development.
Often, the occupational therapist will address sensory processing through observation and interviewing the parents to understand how the child responds to different sensory stimulation. Children with FXS often experience sensory challenges that can interfere with their ability to fully participate and access the early childhood curriculum and learn new skills. Sensory based challenges often are related to poor basic regulation of sleep/wake cycles, feeding and voiding difficulties and the OT can assist in assessment and treatment for these needs. The sensory difficulties are also associated with difficulties with overall behavioral regulation that impacts daily life and learning, so the OT can assist in determining how to best support regulation and coping skills.
- Physical Therapy (PT): PTs can help students develop leisure time interests and assist children who experience fatigue or mobility issues. Gross motor skills in young children with FXS may be impacted by low muscle tone and alignment of the foot or leg during walking and running. The PT can help determine if orthotics, exercise, or positioning will support the developing child’s body so as they grow they don’t develop ongoing difficulties.
- Sensory Integration/Processing Intervention: Sensory integration/processing therapy intervention is most often offered within the licensed oversight of an occupational therapist and may reduce the behavioral symptoms of children that experience hypersensitivity to light, touch, sound, and movement. Sensory difficulties reduce access to learning and access to typical experiences that promote development, so are essential elements to be addressed for young children with FXS. The sensory issues may also be addressed through environmental support at home or school (e.g., adjusting lighting in the classroom, reducing noise level). Occupational therapists can help create overall treatment plans that include environmental supports, interactional supports as well as the direct therapy to remediate the sensory processing difficulties. The OT can also provide sensory supports to proactively help the child to cope and access their world. Such programming should be consistent across home and school environments as well as across the overall intervention plans of the entire team.
Multi-Tiered System of Supports (MTSS) (includes Response to Intervention & Positive Behavior Intervention Supports): One of the most significant shifts in education policy of the past several decades is the implementation of RtI, or Response to Intervention. The reauthorization of the Individuals with Disabilities Education Improvement Act of 2004 (IDEA; P.L. 108-446) allows educators to use responsiveness-to-intervention (RTI) as a substitute for, or supplement to, IQ achievement discrepancy to identify students with learning disabilities (LD) (Fuchs and Fuchs, 2005). MTSS is a framework that evolved out of the RtI and PBIS frameworks that addresses the academic and behavioral needs of students through tiered interventions. The Colorado Department of Education defines MTSS as “A Multi-Tiered System of Supports is a whole-school, prevention-based framework for improving learning outcomes for every student through a layered continuum of evidence-based practices” (Evolution of RtI in Colorado Fact Sheet, January 2014). The belief is that children who are struggling academically may also have some behavioral challenges and conversely, children who have behavioral challenges may also have difficulty learning. Although, males with FXS typically do not qualify for services via a Specific Learning Disability category, this law is very important for females with FXS. Now, the law does not require children to fail prior to receiving intervention(s) to support their learning. MTSS is applied in a variety of forms across the country. Although initially developed as a solution for assessment and diagnosis issues, it also has intervention and behavioral applications. The use of a tiered approach to academic interventions coupled with the significant data collection requirements of this approach are a benefit for children with FXS and should be explored even when an IEP is in place. The graphic below illustrates the primary components of MTSS.
 Related Services: Related services are identified by the Special Education team and found to be necessary for students with disabilities to access their educational curriculum and placement.
Related Services: Related services are identified by the Special Education team and found to be necessary for students with disabilities to access their educational curriculum and placement.
- Safety Plan: This is a plan written for staff to follow in times of emergency such as weather-related disasters, school fires, and acts of violence. Each staff member is directed by this plan to use procedures to evacuate as quickly as possible individuals who are non-ambulatory, nonverbal, hearing or vision impaired, and/or emotionally stressed by the process.
- Health Care Plan: This plan is usually developed by the school nurse who uses medical information provided by outside medical providers. Typically, the health care plan includes medication names, dosages, and side effects. In addition, treatment strategies for specific medical conditions are listed, such as how to deal with a seizure, blood disorders, serious allergies, and use of EpiPen.
- Transportation: IDEA requires that the schools provide transportation from door to school, with specialized equipment as needed, for children receiving special education.
Functional Behavioral Assessment (FBA): An FBA is a problem-solving process, typically conducted by a behavior specialist or school psychologist, designed to determine the underlying cause or function of a specific behavior to determine the best approach for reducing or eliminating the undesired behavior(s). Functions of behavior may include attention or avoidance. During an FBA, professionals should provide direct observation and collect data that may be utilized to complete an ABC chart, which stands for Antecedent, Behavior, and Consequence. Meaning, what happens before (antecedent), during (behavior), and after (consequence). This process will help determine the function or motivation for behavior of the child and the maintaining consequences (Dunlap, et al., 2013).
Applied Behavior Analysis (ABA) Therapy: ABA is not a specific program but rather a behavioral framework from which specific therapeutic interventions (e.g., Lovaas therapy, verbal behavior, discrete trial, etc.) have been developed. As such, there may be wide variability from one ABA program to another. It is important to keep in mind that systematic instruction, careful ongoing assessment, positive reinforcement, and attention to the ABCs (antecedents, behaviors, and consequences) of behavior are essential aspects of any successful therapeutic program, regardless of whether or not it is designated as “ABA.” Decisions about the appropriateness of ABA services for a child with FXS should be made after careful evaluation of the individual. Discrete trial training (DTT) and intensive table teaching (ITT) procedures may need to be less direct and may include another student to utilize peer modeling or turn-taking. Staff working with these students should continue to glean ideas and potential strategies from well-established programs while keeping in mind the syndrome-specific characteristics associated with FXS. One model based on Applied Behavior Analysis that has received much attention due to positive outcomes is the Early Start Denver Model (ESDM), which is an “early intensive and naturalistic developmental behavioral intervention designed specifically for young children 12 to 60 months with or at risk for ASD” (Baril & Humphreys, 2017, p. 322). ABA therapists focus the interventions on the individual needs of the child that may include verbal communication, joint attention (or shared focus between two individuals on an object), and meaningful social interactions with peers and family members. In a recent study, the ESDM was used with parents of young children with FXS (Vismara, McCormick, Shields, & Hessl, 2018) and determined that it is a potentially positive model for parent coaching to improve behavior and skills of their children with FXS.
Alphabet Soup (Important Terms)
ABA Applied behavioral analysis
ABC chart Antecedent, behavior, consequence chart
ASD Autism spectrum disorder
BCBA Board certified behavior analyst
BOCES Board of Cooperative Education Services
BSP Behavior support plan
EI Early intervention
FAPE Free and Appropriate Public Education
FBA Functional behavioral assessment
IDEA Individuals with Disabilities Education Act of 2004
IEP Individualized Education Program
IFSP Individualized Family Service Plan
LEA Lead education agency
LRE Least restrictive environment, a continuum of placements considered, beginning with the general education classroom with neuro-typical peers
MTSS Multi-tiered system of supports
Part B Federal grant to states under IDEA for children aged 3 to 21 years
Part C Federal grant to states under IDEA for children aged birth to 3 years
PBIS Positive behavioral interventions & supports
Procedural safeguards Parental and child rights
RTI Response to intervention
UDL Universal design for learning
Checklist & Strategies
The following may be useful to consider when planning the educational future for the child.
IEP/IFSP Checklist
- Include developmental, functional, academic, and non-academic goals (if needed). These goals are based on the needs defined in the narrative of the IEP/IFSP.
- Limit the number of goals (maximum of five is recommended) because too many can be overwhelming for children, parents, and teachers.
- Use strengths-based language and emphasize the positive, i.e., talk about what the child should do—“use a soft touch”—as opposed to what they should not do—“stop hitting.”
- Write functional, observable, and measurable goals in plain language (i.e., jargon-free) that focus on age appropriate activities that are generalizable across environments, people, and situations.
- If an augmentative communication device or assistive technology is provided, indicate that the equipment will be available for home use and that training should be provided for parents.
- Request that all service providers be present at the IEP meeting. The attendance of a general education teacher is mandated by IDEA (if inclusion services are provided).
- Include all services on the IEP (e.g., speech therapy 30 minutes per week).
- Ask for a draft of the reports prior to the meeting.
- Double-check for inconsistencies within the report.
- Make sure to document who is responsible for both implementing the interventions, as well as who will be responsible for monitoring the progress.
- Provide procedural safeguards, as required, to the parents at the time of the staffing.
Developmental and Educational Strategies for Children with FXS
- Talk, talk, and talk to your child about what is happening during daily routines.
- Follow the CAR Activity:
- Follow their lead in play or storybook reading
- C—Comment on what they are doing/playing
- A—Ask open ended questions
- R—Respond by adding a little bit more
- Wait time—count to yourself up to 10 seconds in between each of these steps
- Incorporate a holistic or simultaneous learning approach (i.e., use a whole word technique rather than a phonics method).
- Include visual cues to help children follow the daily routine in the classroom.
- Teach early math and science concepts using visual and tactile strategies, real object counters, size and shape manipulatives, and concrete examples.
- Teach early literacy skills through everyday literacy tools such as storybooks, environmental print, writing and drawing utensils, pictures, magazines, and oral story telling.
- Incorporate high-interest materials into all areas of the curriculum as needed.
- Use evidence-based interventions within a MTSS framework. These interventions should be based on the phenotypic profile of children with FXS as well as the individual profile of the child. This should include visually based interventions with limited language.
- Use routines based and relationship-based approach. Meaning that predictable routines and positive interactions between adults and children are imperative for healthy development.
- Utilize a family-centered approach.
- Avoid forcing eye contact or using “look at me” prompts.
- Use more commenting than questioning. Reduce direct questions and utilize a fill-in-the-blank format when possible.
- Model and teach play skills. Many children with FXS have dyspraxia, making it challenging to ideate, motor plan, and execute actions. This makes the development of play skills difficult.
References
Baril, E.M. & Humphreys, B.P. (2017). An evaluation of the research evidence on the Early Start Denver Model. Journal of Early Intervention, 39(4), 321-338.
Colorado Department of Education (2014). The evolution of RtI in Colorado. Colorado Multi-Tiered System of Supports (MTSS). CDE Fact Sheet. www.cde.state.co.us/mtss.
Division for Early Childhood. (2015). DEC recommended practices: Enhancing services for children with disabilities and their families (DEC Recommended Practices Monograph Series No. 1). Los Angeles, CA: Author.
Division for Early Childhood (2010). Understanding IDEA: What it means for preschoolers with disabilities and their families. Division for Early Childhood of the Council for Exceptional Children. Missoula, MT: Author.
Dunlap, G., Wilson, K., Strain, P., & Lee, J.K. (2013). Prevent, teach, reinforce for young children: The early childhood model of individualized positive behavior support. Baltimore, MD: Brookes Publishing Co.
Favazza, P.C. & Siperstein, G. N. (2016). Motor skill acquisition for young children with disabilities. In B. Reichow, et al. (Eds.), Handbook of Early Childhood Special Education (pp. 225-245). Switzerland: Springer, DOI 10.1007/978-3-319-28492-7_13
Fuchs, D. & Fuchs, L.S. (2006). Introduction to Response to Intervention: What, why, and how valid is it? Reading Research Quarterly, 93-99, doi:10.1598/RRQ.41.1.4
Individuals with Disabilities Education Act, 20 U.S.C. §1400 (2004).
King, G., Strachan, D., Tucker, M., Duwyn, B., Desserud, S., & Shillington, M. (2009). The application of a transdisciplinary model of early intervention services. Infants & Young Children, 22(3), 211-223.
Lane, J.D. & Brown, J.A. (2016). Promoting communication development in young children with or at risk for disabilities. In B. Reichow, et al. (Eds.), Handbook of Early Childhood Special Education (pp. 199-224). Switzerland: Springer, DOI 10.1007/978-3-319-28492-7_12
Linder, T. W. (2008). Transdisciplinary play-based assessment, 2nd edition. Baltimore, MD: Brookes Publishing Co.
McLean, M. E., Hemmeter, M.L., & Snyder, P. (2014). Essential elements for assessing infants and preschoolers with special needs. Boston: Pearson.
National Research Council. (2008). Early Childhood Assessment: Why, What, and How. Committee on Developmental Outcomes and Assessment for Young Children, C.E. Snow and S.B. Van Hemel, Editors. Board on Children, Youth, and Families, Board on Testing and Assessment, Division of Behavioral and Social Sciences and Education. Washington, DC: The National Academies Press.
Pletcher, L. C. & Younggren, N.O. (2013). The early intervention workbook: Essential practices for quality services. Baltimore, MD: Brookes Publishing Co.
U.S. Department of Health and Human Services & U.S. Department of Education (2015). Policy statement on inclusion of children with disabilities in early childhood program. Washington DC: Author.
Vismara, L.A., McCormick, C.E.B., Shields, R., & Hessl, D. (2018). Extending the parent-delivered Early Start Denver Model to young children with fragile X syndrome. Journal of Autism and Developmental Disorders, https://doi.org/10.1007/s10803-018-3833-1
Author note: This guideline was initially authored by Marcia Braden, Ph.D., Karen Riley, Ph.D., Jessica Zoladz, MS, CGC, Susan Howell, MS, CGC, and Elizabeth Berry-Kravis, M.D., Ph.D., and updated by Jeanine Coleman, Ph.D., and Karen Riley, Ph.D. It was reviewed and edited by consortium members both within and external to the Fragile X Clinical & Research Consortium and it represents the current consensus of the members of the Consortium.
The Fragile X Clinical & Research Consortium was founded in 2006 and exists to improve the delivery of clinical services to families impacted by any Fragile X-associated Disorder and to develop a research infrastructure for advancing the development and implementation of new and improved treatments. Please contact us for more information at 1-800-688-8765.



